The Subtle, Surprising Early Signs of Dementia | Part 2: More Stories + Practical Guidance & Next Steps
Welcome to Part 2 of our comprehensive guide to recognizing early signs of dementia through real family stories.
If you're coming from Part 1, you've already learned about:
Memory and cognitive changes
Behavior and personality shifts
Reasoning, judgment, and safety concerns
Speech and communication changes
You've seen how communication threads through nearly every early sign of dementia, and why speech-language pathologists play such a crucial role in early detection and support.
If you haven't read Part 1 yet, we encourage you to start there: Link to Early Dementia Signs Stories Part 1. It provides essential context, explains the speech-language connection to cognitive changes, and shares the majority of our curated family stories.
In Part 2, You'll Find:
📖 Additional family stories covering sensory changes, emotional shifts, sleep disturbances, movement problems, and the startling phenomenon of confabulation
📋 A comprehensive, printable checklist of early warning signs you can use to document concerns
🏠 Detailed guidance on how in-home speech therapy for dementia with Nina Minervini can help your family at each stage
🎯 Clear action steps for getting professional evaluation and support
💪 Resources and hope for navigating this journey with expert guidance
Let's continue where we left off.
PART 5: Sensory Changes in Taste, Smell & Perception
These changes often start very early, sometimes years before other symptoms become obvious. They're also among the most overlooked signs because they seem unrelated to brain health.
But the olfactory system (smell) and gustatory system (taste) are directly linked to brain regions commonly affected early in Alzheimer's disease, Parkinson's disease, and Lewy body dementia.
Anecdote Spotlight: Son Realizes Something is Wrong
A son said his parent's comment about losing their sense of taste and smell was the moment he realized something deeper was happening. It was the clue that made other small changes suddenly make sense.
Source: https://www.reddit.com/r/AskReddit/comments/1owiser/comment/norklm5/
Clinical Insight
In fact, smell loss is now recognized as one of the earliest detectable signs of neurological decline, sometimes appearing a decade before cognitive symptoms. The olfactory bulb and related brain structures show pathological changes very early in several types of dementia.
Why This Matters
Loss of taste and smell affects:
Nutrition: Food becomes unappetizing, leading to weight loss and poor nutrition
Safety: Can't smell gas leaks, smoke, spoiled food, or other dangerous odors
Quality of life: Food and scents are sources of pleasure and memory
Social engagement: Eating together becomes less enjoyable
The Connection to Communication
While taste and smell might seem unrelated to communication, they're actually deeply connected to:
Memory: Scents trigger powerful memories that support conversation and connection
Emotional processing: Sensory experiences are tied to emotional responses in communication
Social situations: Meals are primary social communication contexts
When these senses decline, the person loses important sensory anchors for memory and emotional connection.
What Families Can Do
Document when taste and smell changes occur
Mention these changes to healthcare providers (they're neurologically significant)
Ensure safety measures are in place (smoke detectors, careful food storage, gas detectors)
Work with professionals to find new ways to make meals engaging and social
PART 6: Emotional and Psychological Shifts
Changes in mental health often precede noticeable memory loss by months or even years. Depression, anxiety, and other emotional symptoms are frequently the first signs that something is changing in the brain.
From a communication perspective, these emotional changes profoundly affect how people engage in conversation and connection with others.
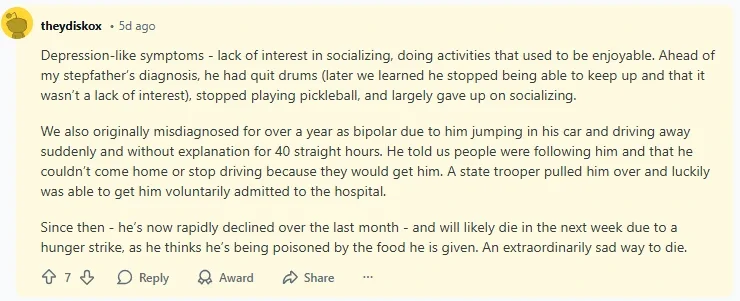
Anecdote Spotlight: Depression Appeared First
A caregiver said depression was the earliest, and most misunderstood, sign of their loved one's dementia. For years before the cognitive symptoms became obvious, their family member had been withdrawn, sad, and unmotivated. Everyone assumed it was just depression. Looking back, it was the beginning of dementia.
Source: https://www.reddit.com/r/AskReddit/comments/1owiser/comment/nosnntk/
Clinical Insight
Depression in older adults can be:
A symptom of early dementia (the brain changes causing dementia also affect mood)
A risk factor for dementia (long-term depression changes the brain in ways that increase dementia risk)
A separate condition that looks like dementia ("pseudodementia")
It's often impossible to know which is which without careful assessment over time.
Why This Is Challenging
The overlap between depression and dementia symptoms makes diagnosis difficult:
Both cause withdrawal from social interaction
Both affect motivation and initiation
Both can impair concentration and memory
Both reduce engagement in previously enjoyed activities
The Communication Impact
Depression dramatically affects communication:
Reduced initiation of conversation
Shorter, less engaged responses
Flat or sad emotional tone
Decreased interest in social connection
Difficulty sustaining conversation
When depression is actually an early sign of dementia, these communication changes persist and worsen despite treatment for depression.
How Speech Therapy Helps
Even when depression and dementia co-occur, speech therapy can:
Provide structured communication opportunities that combat isolation
Use meaningful activities to engage the person despite low motivation
Support family members in maintaining connection when the person is withdrawn
Adapt communication approaches to work with both conditions
Help identify which symptoms are mood-related vs. cognitive
Anecdote Spotlight: Sudden Anxiety
Another person described an abrupt onset of anxiety in someone who had never been anxious before. Their loved one became fearful, worried, and agitated, constantly concerned about things that had never bothered them previously.
Source: https://www.reddit.com/r/AskReddit/comments/1owiser/comment/nosa46u/
Clinical Insight
New-onset anxiety in older adults can signal:
Awareness of cognitive changes (the person senses something is wrong)
Direct neurological effects of dementia on emotional regulation centers
Increased confusion and disorientation causing fear
Loss of ability to problem-solve, making everything feel threatening
What This Looks Like
Common anxiety manifestations in early dementia:
Worry about getting lost or making mistakes
Fear of being alone
Anxiety about forgetting important things
Catastrophic thinking (minor problems feel overwhelming)
Restlessness and inability to settle
The Communication Connection
Anxiety makes communication more difficult because:
The person may avoid situations where they need to communicate
Anxiety interferes with word-finding and processing
Fear of making mistakes leads to reduced speech
Agitation disrupts the flow of conversation
Speech Therapy Approaches for Anxiety
An SLP can help by:
Creating predictable communication routines that reduce uncertainty
Teaching relaxation techniques for use during conversations
Providing communication supports that reduce anxiety-producing situations
Working with family to create calm, supportive communication environments
Identifying and addressing communication-related anxiety triggers
Anecdote Spotlight: Religious Guilt
A loved one developed new, intense guilt centered around religion. They became preoccupied with confessing sins, worried constantly about divine punishment, or expressed fear about their spiritual standing, which were all concerns that seemed disproportionate or unusual for them.
Source: https://www.reddit.com/r/AskReddit/comments/1owiser/comment/nou7dxo/
Clinical Insight
Dementia can amplify fear, guilt, confusion, and intrusive thoughts. The brain loses its ability to:
Regulate obsessive thoughts
Maintain perspective
Reality-test concerns
Self-soothe and find reassurance
This often manifests around topics that were already significant to the person, including religion, family, past mistakes, or responsibilities.
Why This Happens
The frontal lobes help us modulate and regulate repetitive thoughts. When they weaken, thoughts can become:
Repetitive and intrusive
Disconnected from reality
Emotionally overwhelming
Difficult to dismiss or redirect
Communication Challenges
These obsessive concerns dominate conversation:
The person returns to the same worries repeatedly
Reassurance doesn't provide lasting comfort
Conversations get stuck in circular patterns
Family members feel helpless to provide relief
How Speech Therapy Can Address This
While SLPs can't treat the underlying anxiety or obsessive thoughts directly, we can:
Teach validation and redirection techniques
Provide alternative conversation topics and activities
Create structured routines that provide security
Work with family on communication strategies that acknowledge emotions without reinforcing obsessive patterns
Coordinate with mental health professionals for comprehensive care
PART 7: Sleep and Daily Rhythm Changes
Sleep disturbances are extremely common in early dementia, and they significantly impact both the person with dementia and their caregivers. These changes are neurologically based, not just "insomnia."
Anecdote Spotlight: Strange Nighttime Behaviors
A family member became restless at night wandering the house, unable to settle, or engaging in odd activities during hours they should have been sleeping.
Source: https://www.reddit.com/r/AskReddit/comments/1owiser/comment/nort4uc/
Anecdote Spotlight: "I'm Tired but I Can't Sleep"
A caregiver mentioned their loved one expressing exhaustion but being completely unable to fall asleep or stay asleep. This became one of the first clear signs that something was wrong.
Source: https://www.reddit.com/r/AskReddit/comments/1owiser/comment/not7yfu/
Clinical Insight
Circadian rhythm changes are early markers of neurological change. The brain regions that regulate sleep-wake cycles are affected by dementia, leading to:
Difficulty falling asleep
Frequent nighttime waking
Day-night reversal
Sundowning (increased confusion and agitation in late afternoon/evening)
REM sleep behavior disorder (acting out dreams)
The Impact on Daily Life
Sleep disturbances affect everything:
Increased daytime confusion and cognitive impairment
Worsened behavior problems
Caregiver exhaustion
Safety concerns (wandering at night)
Accelerated cognitive decline (poor sleep worsens dementia progression)
The Communication Connection
Sleep-deprived people with dementia experience:
More severe word-finding problems
Increased confusion
Shorter attention spans
Greater frustration and irritability
Reduced ability to engage in conversation
How Speech Therapy Fits In
While sleep management requires medical intervention, speech therapy can help by:
Establishing daytime communication routines that support better day-night differentiation
Providing activities that promote appropriate daytime engagement
Teaching caregivers communication strategies for nighttime restlessness
Working with the care team on comprehensive behavioral approaches
PART 8: Movement, Falls & Physical Red Flags
These signs are often attributed to "bad balance" or "getting older," but they're frequently neurological symptoms that warrant attention.
Anecdote Spotlight: Early Falls
A data scientist noticed during a study that having a medical code for falling often was often an indicator.
Source: https://www.reddit.com/r/AskReddit/comments/1owiser/comment/norky0u/
Anecdote Spotlight: Another Fall Pattern
Another user described the same pattern. Their mother was falling without a clear cause, happening repeatedly, with no obvious environmental hazard.
Source: https://www.reddit.com/r/AskReddit/comments/1owiser/comment/norq7v4/
Clinical Insight
Falls often precede cognitive decline in several dementia types:
Vascular dementia: Small strokes affect balance and coordination
Lewy body dementia: Movement symptoms appear early, similar to Parkinson's
Parkinson's disease dementia: Motor symptoms typically come first
Normal pressure hydrocephalus: A triad of gait problems, incontinence, and cognitive decline
Why Movement Matters for Communication
Movement and communication are more connected than most people realize:
Speech requires precise motor control
Swallowing safety depends on motor coordination
Facial expressions rely on motor function
Gesture and body language support verbal communication
When movement systems are affected early, speech and swallowing often follow.
What Speech Therapists Watch For
Falls may coincide with:
Changes in speech clarity or voice quality
Reduced facial animation
Swallowing difficulties
Less use of gesture
Reduced prosody (flat, monotone speech)
The Comprehensive Evaluation
When falls are present, speech-language pathologists conduct thorough assessments of:
Speech motor control
Swallowing safety (dysphagia screening)
Voice quality and breath support
Oral motor coordination
Early identification allows for preventive strategies before aspiration or malnutrition become concerns.
PART 9: Alcohol, Eating & Routine Self-Care
Loss of routine can be dramatic and dangerous. These changes often signal that executive function, or the brain's ability to plan, monitor, and regulate behavior, is breaking down.
Anecdote Spotlight: Alcoholism Emerging or Becoming Visible
A loved one who had never seemed to have a drinking problem suddenly couldn't hide their alcohol use. What may have been quiet drinking became obvious excess, or the person who previously drank moderately lost the ability to regulate their consumption.
Source: https://www.reddit.com/r/AskReddit/comments/1owiser/comment/notpeka/
Clinical Insight
This can reflect:
Loss of impulse control (can't stop after one drink)
Loss of social awareness (drinking at inappropriate times)
Loss of judgment (unable to recognize when drinking is excessive)
Use of alcohol to self-medicate confusion or anxiety
Memory loss (forgetting how much they've already consumed)
The Danger
Alcohol accelerates cognitive decline and interacts dangerously with many medications. It also increases fall risk, poor nutrition, and social problems.
Speech Therapy Considerations
Alcohol use complicates communication and therapy because it:
Affects speech clarity and motor control
Impairs memory and learning
Reduces engagement and motivation
May indicate unaddressed emotional needs
A comprehensive approach requires addressing both the cognitive changes and the substance use with appropriate medical and behavioral support.
Anecdote Spotlight: Forgetting to Eat
A commenter shared that their loved one simply stopped eating regularly because they "forgot" to eat. They'd skip meals without realizing it, lose weight, and seem genuinely surprised when asked if they'd had lunch.
Source: https://www.reddit.com/r/AskReddit/comments/1owiser/comment/nov0nyd/
Clinical Insight
Multiple factors contribute to this:
Loss of hunger signals (the brain doesn't register the need to eat)
Memory loss (can't remember whether they've eaten)
Loss of routine (no structured meal schedule)
Apraxia (difficulty planning and executing the steps of meal preparation)
Depression (reduced motivation and pleasure in eating)
The Health Consequences
Malnutrition develops quickly and causes:
Accelerated cognitive decline
Increased fall risk
Weakened immune system
Further weight loss and frailty
Reduced quality of life
How Speech Therapy Addresses Eating
This is a core area of speech-language pathology expertise. We assess and treat:
Swallowing safety: Is the person at risk for aspiration?
Oral motor function: Can they chew and manipulate food safely?
Cognitive aspects of eating: Can they sequence the steps of a meal?
Environmental supports: What modifications help support eating?
Practical Interventions
An SLP can help by:
Conducting swallow evaluations to ensure safety
Recommending diet textures that are safe and appealing
Creating visual schedules and reminders for meals
Teaching caregivers mealtime communication strategies
Making meals a social, engaging activity rather than just a task
Monitoring for aspiration risk as cognitive decline progresses
PART 10: Bizarre or Impossible Stories (Confabulation)
One of the most jarring early signs is when a person begins confidently telling stories that never happened. This is called confabulation, and it's fundamentally different from lying.
Anecdote Spotlight: Fantasies Reported as Reality
A caregiver described their loved one telling detailed, elaborate stories that were clearly imaginary, but the person telling them believed they were completely true. They'd describe events that couldn't possibly have happened with absolute conviction.
Source: https://www.reddit.com/r/AskReddit/comments/1owiser/comment/noqesap/
Anecdote Spotlight: Truly Bizarre Stories
Another commenter mentioned stories that were extremely dark, making claims about things that defied reality, told as if they were ordinary events.
Source: https://www.reddit.com/r/AskReddit/comments/1owiser/comment/nose2fo/
Clinical Insight
Confabulation is not lying; it's the brain trying to fill in gaps in memory with plausible (or sometimes implausible) explanations. The person genuinely believes what they're saying.
This happens because:
Memory gaps are uncomfortable, so the brain fills them in
The frontal lobes (which help us monitor the accuracy of our thoughts) are weakening
The person loses the ability to distinguish real memories from imagined scenarios
They can't reality-test their own narratives
What This Looks Like
Common confabulation patterns:
Describing visits from people who didn't visit
Reporting trips or activities that didn't happen
Creating explanations for missing objects or time gaps
Combining elements from different time periods into one story
Inserting themselves into news stories or others' experiences
Why This Is Distressing for Families
Confabulation is emotionally difficult because:
It feels like the person is lying (they're not)
Correcting them doesn't help and often causes conflict
The stories can be bizarre or upsetting
It signals that reality is becoming unstable for the person
The Speech Therapy Approach
As communication specialists, speech-language pathologists can help families navigate confabulation by:
Teaching validation techniques: Instead of correcting the false story, we validate the underlying emotion or need. For example:
Person with dementia: "I had lunch with Mom today" (Mom passed away years ago)
Unhelpful response: "No, you didn't. Mom is dead. Remember?"
Helpful response: "You're thinking about Mom. You must miss her. Tell me about her."
Identifying patterns: Sometimes confabulation reveals unmet needs. A person who repeatedly describes imaginary visitors might be lonely. Someone who insists they need to "go to work" might need a sense of purpose.
Preserving dignity: We help families respond in ways that:
Don't humiliate or embarrass the person
Maintain the relationship and trust
Reduce anxiety and distress
Support whatever reality the person is experiencing
Creating memory supports: For confabulation driven by memory gaps, we can:
Provide memory books with accurate information
Create visual timelines
Use photos and documentation to gently ground the person
Establish predictable routines that reduce uncertainty
PART 11: When Dementia Isn't Alzheimer's
Most people think "dementia" means "Alzheimer's disease," but Alzheimer's is actually just one type of dementia. There are many others, and they often present with different early warning signs.
Understanding the differences matters because:
Different dementias progress differently
Treatment approaches vary
Some are more treatable than others
Knowing the type helps families know what to expect
Lewy Body Dementia (LBD)
Early signs that suggest LBD:
Visual hallucinations (seeing people, animals, or objects that aren't there)
Movement problems similar to Parkinson's disease (tremor, stiffness, slow movement)
Severe sleep disturbances, especially acting out dreams (REM sleep behavior disorder)
Fluctuating cognition (good days and bad days with dramatic differences)
Extreme sensitivity to antipsychotic medications
Speech therapy is particularly important in LBD because:
Speech and swallowing problems develop earlier than in Alzheimer's
Voice becomes softer and less clear
Facial expression reduces (masked face)
Swallowing difficulties require close monitoring
Vascular Dementia
Early signs that suggest vascular dementia:
Stepwise decline (sudden drops in function rather than gradual decline)
History of strokes or transient ischemic attacks (TIAs)
Early problems with executive function (planning, organizing, problem-solving)
Mood changes, especially depression or emotional lability
Gait problems and falls
Speech therapy considerations:
Language problems may be more focal (specific areas affected)
May have more preserved memory initially
Executive dysfunction affects communication planning
Swallowing problems may develop suddenly after strokes
Frontotemporal Dementia (FTD)
Early signs that suggest FTD:
Personality changes and behavior problems appear before memory loss
Loss of empathy and social awareness
Inappropriate behavior, impulsivity, or apathy
Language problems (difficulty speaking or understanding)
Compulsive behaviors or rituals
Tends to affect people younger than Alzheimer's (typically 45-65 years old)
Speech therapy is crucial in FTD because:
Language problems are often the primary symptom
Two variants specifically affect language:
Progressive nonfluent aphasia: Difficulty producing speech, grammar problems
Semantic dementia: Loss of word meaning, can't name objects
Communication breakdown happens earlier and more severely
Behavioral changes dramatically affect social communication
Why Accurate Diagnosis Matters
Different dementia types respond differently to:
Medications (some drugs that help Alzheimer's may worsen other types)
Behavioral interventions
Communication strategies
Safety planning
Getting an accurate diagnosis early allows for:
Appropriate medical management
Targeted speech therapy interventions
Better family education and preparation
Connection to type-specific support resources
Your Comprehensive Early Warning Signs Checklist
If you notice multiple signs across categories, not just one isolated incident, consider seeking a comprehensive evaluation including speech-language assessment.
Print this checklist and keep track of what you're noticing over time. Bring it with you to medical appointments.
Memory & Thinking
□ Repeating questions within the same conversation
□ Getting lost in familiar places
□ Forgetting recent actions (whether they've eaten, taken medication, or completed tasks)
□ Difficulty learning new information or routines
□ Losing track of dates, seasons, or the passage of time
Behavior & Personality
□ Uncharacteristic irritability or anger
□ Sudden mood swings or emotional outbursts
□ Unusual changes in personality (becoming nicer or meaner)
□ New "quirky" behaviors or rituals
□ Withdrawal from social activities or hobbies
□ Ability to "mask" problems in public while family sees struggles at home
Reasoning, Judgment & Safety
□ Poor decisions, especially with money
□ Difficulty with familiar tasks (can't work common objects)
□ Problems with planning or organizing
□ Misplacing things in unusual locations
□ Falling for scams or being manipulated
□ Unsafe behaviors (leaving stove on, getting lost while driving)
Communication & Language
□ Difficulty finding words (more than normal "tip of the tongue")
□ Using simpler, shorter sentences than before
□ Repeating the same phrases, questions, or stories
□ Subtle changes in speech rhythm, clarity, or tone
□ Trouble following conversations, especially in groups
□ Difficulty understanding complex explanations or instructions
□ Reduced participation in conversation
Sensory Changes
□ Loss of taste or smell
□ Changes in visual perception
□ Difficulty judging distances or spatial relationships
Emotional & Psychological
□ New or worsening depression
□ Sudden onset of anxiety or fearfulness
□ Obsessive worries or repetitive concerns
□ Religious guilt or preoccupation
□ Paranoia or suspiciousness
Sleep & Daily Rhythms
□ Difficulty falling or staying asleep
□ Restlessness or wandering at night
□ Excessive daytime sleepiness
□ Confusion or agitation in the evening (sundowning)
Movement & Physical Function
□ Unexplained falls or balance problems
□ Stiffness, tremor, or slowed movement
□ Changes in gait or walking pattern
□ Reduced facial expression
Daily Routines & Self-Care
□ Changes in alcohol use or loss of control over drinking
□ Forgetting to eat or eating excessively
□ Poor hygiene or grooming (when this was never an issue)
□ Medication errors (too much, too little, or forgetting)
□ Difficulty managing finances or paying bills
Confabulation & Reality Testing
□ Telling detailed stories about events that didn't happen
□ Confusing dreams with reality
□ Misidentifying people or places
□ Believing things that aren't true with strong conviction
Swallowing & Eating Safety
□ Coughing or choking during meals
□ Wet or gurgly voice after eating or drinking
□ Avoiding certain food textures
□ Taking much longer to finish meals
□ Unexplained weight loss
Tracking Changes Over Time
Keep a journal or notes documenting:
Date and time of concerning incidents
What happened specifically
Context (where, when, who was present)
Frequency (first time, occasional, or frequent)
Your loved one's reaction (aware, confused, frustrated, unconcerned)
This documentation helps healthcare providers understand patterns and make accurate diagnoses.
How In-Home Speech Therapy Can Help | Nina Minervini's Approach
Now that you understand the wide range of early signs and how deeply communication is affected by dementia, let's talk about what you can actually do about it.
This is where specialized speech therapy makes a profound difference, and it’s where working with an experienced clinician like Nina Minervini in the comfort of your own home can change the trajectory of your family's journey with dementia.
Why Speech Therapy Matters in Dementia Care
Many families don't realize that speech-language pathologists are experts in cognitive-communication disorders. We don't just treat speech sounds or stuttering. We specialize in how the brain processes, organizes, and expresses language and thought.
When dementia affects the brain, it affects:
Memory for conversations, names, recent events
Language — finding words, forming sentences, understanding complex information
Attention — staying focused during conversation, processing what others say
Executive function — planning what to say, organizing thoughts, sequencing ideas
Social communication — reading social cues, understanding implied meaning, maintaining relationships through conversation
Swallowing — coordinating the complex motor and cognitive processes required for safe eating
Speech therapy addresses ALL of these areas.
Compassionate, Comprehensive In-Home Care
Nina specializes in working with adults experiencing cognitive-communication changes, including those in the early and middle stages of dementia. Her approach is grounded in:
1. Thorough Assessment
Before beginning intervention, Nina conducts comprehensive evaluation of:
Current communication strengths and challenges
Memory and cognitive function as they affect communication
Swallowing safety
Daily communication needs and goals
Family communication patterns and concerns
Environmental factors affecting function
This assessment creates a clear baseline and identifies the most important areas to address.
2. Meaningful, Functional Goals
Nina doesn't focus on abstract exercises. Goals center on what matters most to your family:
"Help Dad participate in family dinners without getting frustrated"
"Enable Mom to continue her daily phone calls with her sister"
"Support safe medication management through communication strategies"
"Maintain connection through conversation despite memory loss"
"Ensure safe swallowing as cognitive changes progress"
3. Strategies That Work in Real Life
Interventions are practical and immediately applicable:
Memory supports: Visual schedules, memory books, labeled photos, reminder systems
Communication strategies: Simplified language, yes/no questions, visual supports, validation techniques
Environmental modifications: Reduced distractions, clear signage, organized spaces
Caregiver training: Teaching family members techniques that reduce frustration and maintain connection
Swallow safety: Diet modifications, safe feeding strategies, monitoring for aspiration risk
4. Support Across the Journey
Nina understands that dementia is progressive. Her approach includes:
Regular re-evaluation as needs change
Adjusting strategies as the person's abilities evolve
Preparing families for what's ahead
Connecting families with additional resources
Providing compassionate support during difficult transitions
5. Collaboration With Your Care Team
Nina works closely with:
Physicians and neurologists
Occupational and physical therapists
Social workers and case managers
Memory care programs
Home health agencies
This collaborative approach ensures comprehensive, coordinated care.
Take the First Step: Get Started with Nina Minervini
If you've recognized your loved one in any of these stories, and if you've been noticing small changes that worry you, if conversations feel different, if you're seeing early warning signs, now is the time to seek help. Advanced senior care for speech therapy can come right to your doorstep.
Why You Shouldn't Wait
Every day without support is a day of:
Unnecessary frustration for both you and your loved one
Missed opportunities for meaningful connection
Potential safety risks going unaddressed
Communication decline that could have been slowed
Caregiver stress that could have been reduced
The families who look back and say "I wish we'd started sooner" are the ones who waited until problems became severe. Don't let that be your story.
What Happens When You Reach Out
Step 1: Initial Consultation
Nina will talk with you about what you're noticing, your concerns, and your loved one's history. This conversation helps determine whether speech therapy would be beneficial and what to expect.
Step 2: Comprehensive Evaluation
Nina comes to your home to conduct a thorough assessment. This includes:
Cognitive-communication evaluation
Swallowing screening if indicated
Observation of daily routines and interactions
Discussion with family members about specific concerns
Review of medical history and current medications
Step 3: Personalized Treatment Plan
Based on the evaluation, Nina develops a customized plan targeting:
Your family's specific goals and priorities
Your loved one's individual strengths and challenges
Practical strategies you can use immediately
Long-term planning for changes ahead
Step 4: Regular Therapy Sessions
Nina provides ongoing in-home therapy sessions focused on:
Skill-building and strategy implementation
Family training and coaching
Environmental modifications
Monitoring for changes
Adjusting approaches as needs evolve
Step 5: Ongoing Support
You'll have access to Nina for questions, concerns, and guidance as you navigate this journey together.
Ready to Get Started? Contact Nina Minervini Today
📞 Phone: (561) 797-2343
📧 Email: ninaminervini11@gmail.com
🌐 Contact Form
About This Series
This two-part article series brings together real stories from families who've experienced the early stages of dementia, paired with clinical insights to help other families recognize warning signs sooner.
Part 1 covered memory changes, behavior shifts, reasoning problems, and early speech changes.
Part 2 (this article) covered sensory changes, emotional shifts, sleep disturbances, movement problems, eating changes, confabulation, different dementia types, and comprehensive guidance for seeking help.
All family anecdotes come from public forums where caregivers generously shared their experiences. Clinical insights are provided by speech-language pathology professionals specializing in cognitive-communication disorders.
If you found this series helpful, please share it with others who might be noticing early signs in their loved ones. Early recognition saves families unnecessary suffering and opens doors to interventions that truly make a difference.
For the complete picture, be sure to read Part 1 if you haven't already.
Frequently Asked Questions
"Isn't it too early to worry about this?"
If you're noticing multiple warning signs, it's not too early. Early intervention provides the best opportunity for maintaining function and quality of life. It's always better to evaluate and find out you're being cautious than to wait and miss the window for effective intervention.
"Will speech therapy cure dementia?"
No. Dementia is a progressive condition, and speech therapy cannot reverse it. However, speech therapy can:
Slow the rate of communication decline
Maintain abilities longer
Teach compensatory strategies
Ensure swallowing safety
Significantly improve quality of life for both the person with dementia and their family
Provide support and guidance throughout the journey
"My loved one can still talk. Why do they need speech therapy?"
Speech therapy for dementia isn't just about talking. It addresses:
Memory for conversations
Finding the right words
Following directions
Staying on topic
Problem-solving through conversation
Swallowing safety
Family communication training
Many of these areas are affected long before obvious speech problems appear.
"How long does speech therapy take?"
It varies based on the stage of dementia and individual needs. Some families benefit from:
Short-term intensive intervention to establish strategies
Ongoing periodic sessions to adjust approaches as needs change
Consultation as needed for specific concerns
Nina will work with you to develop a plan that makes sense for your family's situation and goals.
"Does insurance cover in-home speech therapy?"
Many insurance plans, including Medicare, cover medically necessary speech therapy for cognitive-communication disorders and swallowing problems. Nina's office can help you understand your benefits and handle insurance paperwork.
Coverage details vary, so it's best to call and discuss your specific situation.
"What if my loved one refuses help?"
This is common, especially in early stages when the person may not recognize their difficulties. Nina has extensive experience working with reluctant clients and can often help by:
Framing therapy as support for something specific they care about
Starting with very non-threatening activities
Building rapport and trust gradually
Working with family members first, then involving the person incrementally
Sometimes the initial evaluation itself helps the person recognize that support would be beneficial.
"We already have so many appointments. Is this really necessary?"
Communication is fundamental to everything: relationships, safety, daily functioning, quality of life. When communication breaks down, everything becomes harder. Speech therapy often reduces problems in other areas by improving the foundation: how you connect and communicate with each other.
Many families find that speech therapy actually reduces stress and makes other aspects of care easier.
"What's the difference between in-home therapy and clinic-based therapy?"
In-home therapy provides:
Assessment and treatment in the person's natural environment
Observation of real-life challenges
Immediate application to daily routines
Family training in the actual situations where strategies are needed
Greater comfort for people who are anxious in medical settings
No transportation challenges
For people with dementia, the home environment provides crucial context that a clinic cannot.