The Subtle, Surprising Early Signs of Dementia 🧠 Part 1: Real Family Stories
For many families, dementia doesn't announce itself with the dramatic memory loss we see in movies. It doesn't start with someone forgetting their own name or the faces of their children.
Instead, it begins quietly: in a shift of tone during conversation, a strange moment of confusion in a familiar place, a forgotten task that was routine for decades, or a story that doesn't quite make sense.
These early signs are easy to dismiss. We tell ourselves it's stress, normal aging, or just a personality quirk. We make excuses because the alternative feels too frightening to consider.
But when families look back after a diagnosis, many realize the same thing:
"The signs were there. We just didn't know what they meant."
About This Two-Part Series
This article is Part 1 of a comprehensive two-part series designed to help families recognize the early warning signs of dementia through real stories shared by caregivers and loved ones.
In Part 1 (this article), you'll find:
Real family stories from people who've watched dementia unfold
Clinical explanations of what these early signs mean
How communication and speech are affected by cognitive changes
The majority of our curated anecdotes organized by category
Coming in Part 2:
Additional family stories and warning signs
A comprehensive, printable early signs checklist
Detailed guidance on how in-home speech therapy can help
Practical strategies and next steps for families
Resources for getting professional support
Each story in this series comes from a Reddit thread where families openly shared the first clues they noticed, maybe ones they wish they'd understood sooner, patterns they wish they'd recognized before communication became more difficult.
Hopefully, these voices can help someone else recognize the early stages in time to seek support, including specialized speech therapy for dementia and Alzheimer’s that can make a meaningful difference in quality of life and family connection.
Why Communication Changes Matter: The Speech-Language Connection
Before we dive into the stories families have shared, it's important to understand something crucial: many of the earliest signs of dementia involve language, communication, and the cognitive processes that support them.
A trained and experienced speech-language pathologist is uniquely positioned to recognize these early changes because we're trained to notice subtle shifts in:
Word-finding abilities
Sentence complexity and structure
Conversational turn-taking
Understanding of abstract language
Memory for spoken information
Ability to follow multi-step directions
Social communication and pragmatic language skills
When families notice that "something seems off" in how their loved one communicates, they're often picking up on neurological changes that affect language processing, memory, attention, and executive function, and these are all areas where speech therapy can provide targeted intervention and support.
Throughout this article, you'll see how communication changes weave through nearly every early sign of dementia. Understanding this connection can help families seek appropriate help sooner.
PART 1: Memory and Cognitive Changes
The media often frames dementia as "forgetting names" or "not remembering yesterday." But for many families, the earliest signs involve patterns, not single moments, that include changes in how a person thinks, plans, remembers, or orients themselves in familiar environments.
These early cognitive shifts are often subtle, but deeply meaningful. And many of them directly impact a person's ability to communicate effectively.
🧠 Anecdote Spotlight: Asking the Same Questions, Like a Scripted Conversation
A family member shared how their mother began asking the same questions and repeating the same conversation prompts every time they saw her. What made this particularly poignant was that she wasn't doing this because she had forgotten their last conversation: she was doing it deliberately.
Her repeated questions had become a script, a carefully developed strategy to cover up her memory loss and confusion. The family member noted how surprising it was to realize how quickly their mom had developed this coping mechanism to mask the signs of her cognitive decline.
Source: https://www.reddit.com/r/AskReddit/comments/1owiser/comment/norfuoy/
Clinical Insight
Short-term memory is usually the first system affected in dementia. Repeating questions is not just "forgetfulness.” It reflects an inability to store or retrieve new information that was just provided. The information enters the brain but doesn't get consolidated into memory, so from the person's perspective, they're asking for the first time, every single time.
How Speech Therapy Helps
A speech-language pathologist can assess the specific nature of the memory deficit and teach compensatory strategies that work with the person's remaining strengths. This might include:
Creating memory aids and visual supports tailored to the individual
Teaching family members communication strategies that reduce the need for repeated questions
Establishing predictable routines that provide security and reduce anxiety
Using external memory systems (calendars, notebooks, photo albums) to support conversation
🧠 Anecdote Spotlight: Getting Lost in Familiar Places
One commenter shared that their family member began getting lost while navigating places they'd known for decades. Other long-time habits began to shift, and additionally, similar to the previous anecdote, some habits changed as a strategy to mask deficits with loved ones.
Source: https://www.reddit.com/r/AskReddit/comments/1owiser/comment/not48zp/
Clinical Insight
Spatial memory, route planning, and orientation decline early in many types of dementia. The brain regions responsible for creating mental maps and following familiar routes begin to deteriorate. This is why dementia can mimic "poor navigation skills" or "confusion" at first, but it's actually a neurological change affecting visual-spatial processing.
The Communication Connection
Getting lost often goes hand-in-hand with difficulty describing locations, following directional language ("turn left at the corner"), and understanding spatial prepositions ("the keys are on the table beside the lamp"). These language-based navigation skills are intertwined with spatial memory.
🧠 Anecdote Spotlight: Forgetting They Already Drank
A parent who normally had one glass of wine with dinner began drinking entire bottles, because they kept forgetting they'd already poured and finished a glass. The family initially thought it was intentional until they realized their loved one genuinely had no memory of drinking.
Source: https://www.reddit.com/r/AskReddit/comments/1owiser/comment/nori4tp/
Clinical Insight
This represents a dangerous combination: loss of episodic short-term memory mixed with impaired judgment. The person can't remember the action they just completed, and they've also lost the ability to monitor their own behavior or recognize when something is wrong.
The Safety Concern
This same pattern can apply to medications, food, or any repeated action. Without intervention, it becomes a significant safety risk.
How Speech Therapy Addresses This
Speech-language pathologists work on developing systems to support sequenced tasks and routine monitoring. This might include:
Visual checklists with checkboxes for daily tasks
Medication management systems with clear visual cues
Training caregivers to provide gentle reminders without creating conflict
Structured mealtime routines that prevent over-eating or under-eating
🧠 Anecdote Spotlight: Mistaking Loved Ones for Other People
A family member began confusing close relatives with acquaintances or strangers. They might call their daughter by their sister's name, fail to recognize their son-in-law despite decades of family dinners together, or in this case, begin mixing up their grandchildren.
Source: https://www.reddit.com/r/AskReddit/comments/1owiser/comment/nostzge/
Clinical Insight
This reflects early changes in facial recognition, social memory, and contextual awareness. The brain struggles to retrieve stored information about familiar people or to match a face with the correct identity. It's not that the person doesn't care; their brain is literally unable to make the connection.
How This Affects Communication
When someone can't remember who they're talking to, conversation becomes fragmented and confusing. They might share inappropriate information (telling a story meant for a close friend to a casual acquaintance), or they might become anxious and withdrawn because they're embarrassed about not recognizing someone they should know.
Speech Therapy Interventions
A speech-language pathologist can help by:
Teaching caregivers to provide contextual cues ("Hi Dad, it's me, Sarah, your daughter")
Creating photo books with names and relationships clearly labeled
Developing conversation strategies that don't rely on remembering names or relationships
Supporting emotional regulation when confusion causes distress
PART 2: Behavior and Personality Shifts
Many families notice behavior changes long before obvious memory problems emerge. These can be subtle shifts in tone, temperament, or judgment, which are all changes that make you think, "That's not like them."
For speech-language pathologists, these changes are significant because personality and behavior are deeply connected to pragmatic language skills: the social rules of communication, emotional regulation during conversation, and the ability to navigate complex social situations.
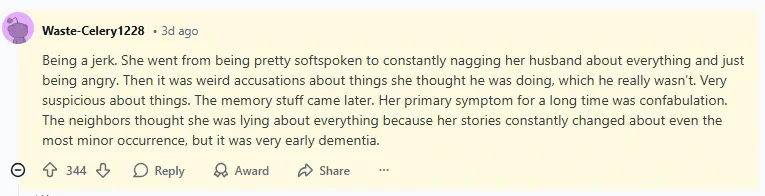
🧠 Anecdote Spotlight: "He Just Became a Jerk"
A commenter said their normally kind, patient, and gentle loved one became irritable, short-tempered, and mean seemingly out of nowhere. The person who used to be the peacemaker in the family started picking fights and saying hurtful things.
Source: https://www.reddit.com/r/AskReddit/comments/1owiser/comment/noqwj34/
Clinical Insight
The frontal lobes, which are responsible for emotional regulation, impulse control, and social behavior, often weaken early in dementia. When these brain regions deteriorate, people lose the ability to filter their thoughts before speaking, regulate their emotional responses, or consider how their words affect others.
The Communication Impact
This personality shift fundamentally changes family communication. Conversations that used to be pleasant become tense. Family members start walking on eggshells. The person with dementia may not understand why everyone seems upset with them.
How Speech Therapy Can Help
While speech therapy can't reverse the underlying neurological changes, it can:
Help family members understand that the irritability is a symptom, not a choice
Teach communication strategies that reduce triggers for outbursts
Provide de-escalation techniques for tense moments
Support the person with dementia in expressing needs and emotions more effectively
Facilitate family communication training so everyone can adapt their approach
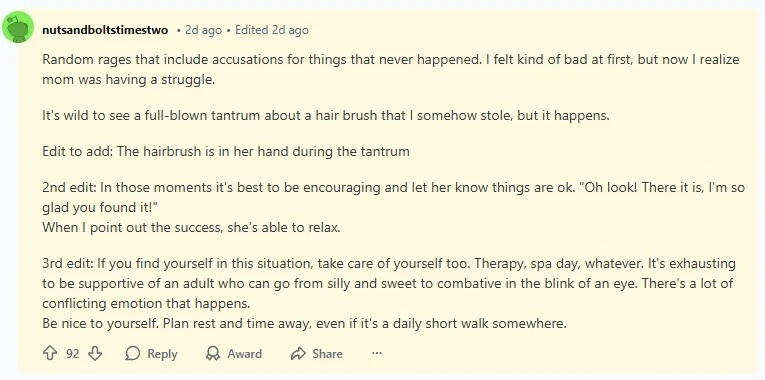
🧠 Anecdote Spotlight: Random Rages
A peaceful, easy-going family member began exploding in anger with no clear triggers. One moment they'd be calm, the next moment they'd be yelling about something minor or seemingly nothing at all. Included in this anecdote is some first-hand advice for caregivers dealing with these situations.
Source: https://www.reddit.com/r/AskReddit/comments/1owiser/comment/noro4nr/
Clinical Insight
Loss of impulse control and decreased frustration tolerance are early markers in multiple dementia types, particularly frontotemporal dementia and vascular dementia. The "pause button" that helps most of us regulate emotional reactions stops working properly.
Understanding the Trigger
Often, these seemingly random rages do have triggers, but they're related to internal experiences the person can't articulate. They might be:
Frustrated by their own cognitive difficulties
Unable to express a physical need (pain, hunger, bathroom needs)
Overwhelmed by environmental stimulation
Confused about where they are or what's happening
The Speech Therapy Approach
A speech-language pathologist specializing in cognitive-communication disorders can:
Assess whether communication difficulties are triggering frustration
Teach the person alternative ways to express needs and emotions
Help caregivers recognize early signs of escalation
Develop communication strategies that validate feelings while redirecting attention
Create calm, structured communication environments that reduce overwhelm
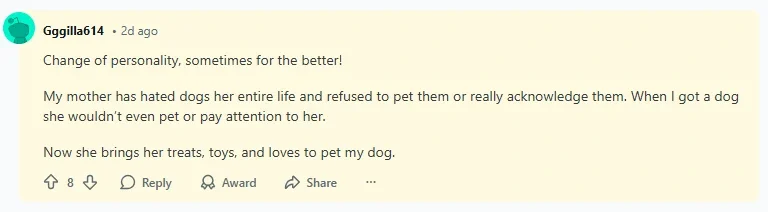
🧠 Anecdote Spotlight: Surprisingly, Becoming Nicer
One caregiver said their loved one actually became kinder, more pleasant, and easier to get along with as dementia began. A person who had been somewhat critical or anxious their whole life became gentle and agreeable.
Source: https://www.reddit.com/r/AskReddit/comments/1owiser/comment/not0jgm/
Clinical Insight
Not all personality changes go in a negative direction. Loss of inhibition can flatten previous anxiety, worry, or irritability. Some people lose the critical filter that made them seem harsh, while others lose the anxiety that kept them on edge. In some cases, the simplification of thought processes actually brings a kind of peace.
Why This Matters
This is a perfect example of why families need to pay attention to any uncharacteristic change, not just negative ones. A dramatic shift in any direction suggests neurological changes are occurring.
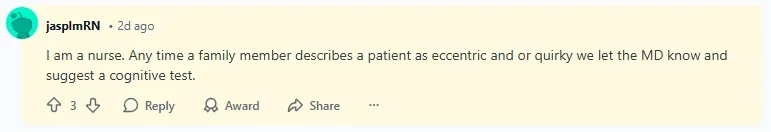
🧠 Anecdote Spotlight: "Eccentric" or "Quirky" Behavior
A healthcare professional wrote that early signs seemed like harmless quirks: odd habits, weird decisions, unusual new routines that the family wrote off as "just something they're doing now." However, with years of experience, they now take “quirky” as a possible sign of underlying issues.
Source: https://www.reddit.com/r/AskReddit/comments/1owiser/comment/notv20f/
Clinical Insight
Families often rationalize early symptoms as personality changes, hobbies, or harmless eccentricities. But when quirks accumulate and intensify, they're often signs of executive dysfunction: the brain's ability to plan, organize, and regulate behavior is weakening.
The Pattern to Watch For
One odd behavior might be nothing. But when you start seeing multiple new quirks, especially if they're:
Repetitive or ritualistic
Disconnected from the person's previous interests
Interfering with daily functioning
Accompanied by other subtle changes
...it's time to pay closer attention.
🧠 Anecdote Spotlight: Masking the Symptoms
A commenter shared their father's experience with cognitive decline, noting what consistently surprised them most: their father didn't panic about his deteriorating condition. Even as he forgot what certain towns were or seemed to lose awareness of basic things, he didn't appear worried.
When taking their father to doctors and psychologists, he would "act completely normal," despite the fact that he was experiencing significant confusion and couldn't operate most things in his daily life.
Source: https://www.reddit.com/r/AskReddit/comments/1owiser/comment/noub1nx/
Clinical Insight
Early dementia often involves preserved social scripts and automatic responses. People can rely on decades of learned social behaviors to navigate brief interactions. They might be able to make small talk, laugh at appropriate moments, and maintain a pleasant demeanor all while struggling significantly with actual cognitive tasks.
This is why doctors sometimes miss early dementia in office visits. The person seems "fine" in a brief, structured interaction.
Why Speech Therapists Recognize This
Speech-language pathologists are specifically trained to look beyond surface-level communication and assess deeper processing abilities. We use structured assessments that go beyond social chitchat to reveal underlying difficulties with:
Complex language comprehension
Problem-solving through conversation
Following multi-step instructions
Processing abstract concepts
Maintaining attention across longer discourse
PART 3: Reasoning, Judgment & Safety Concerns
Some of the first signs of dementia involve changes in problem-solving, sequencing, and basic safety awareness. These often manifest as small mistakes that seem inconsequential at first, that is, until they accumulate or escalate into dangerous situations.
From a speech therapy perspective, many of these changes reflect executive dysfunction: the brain's ability to plan, sequence, and complete multi-step tasks is breaking down.
🧠 Anecdote Spotlight: Couldn't Latch a Seatbelt
Someone who had driven their entire life, someone who had buckled a seatbelt thousands of times, suddenly couldn't figure out how to do it. They held the buckle, stared at it, and couldn't sequence the simple motor movements required to click it into place.
Source: https://www.reddit.com/r/AskReddit/comments/1owiser/comment/notjzye/
Clinical Insight
This reflects impaired motor planning, also called apraxia, a major early sign of dementia. The person knows what they want to do, but their brain can't send the correct signals to coordinate the movement. This is particularly concerning when it involves deeply ingrained, automatic tasks.
The Speech Therapy Connection
Apraxia doesn't just affect movement; it affects speech production too. Many people with dementia develop apraxia of speech, where they struggle to coordinate the movements needed for clear speech even though their muscles are physically fine.
What Speech Therapy Offers
A speech-language pathologist can:
Assess for both limb apraxia and speech apraxia
Develop compensatory strategies for communication when speech becomes effortful
Teach caregivers to recognize when the person is struggling with motor planning, not being stubborn
Introduce alternative communication methods if speech apraxia progresses
🧠 Anecdote Spotlight: Frozen Food in the Fridge
An otherwise capable parent began putting frozen items in the refrigerator instead of the freezer. At first, this odd behavior was chalked up to the fact that this older gentleman rarely took part in household tasks, but it was only the first in many signs that something else was happening.
Source: https://www.reddit.com/r/AskReddit/comments/1owiser/comment/notucjx/
Clinical Insight
Dementia disrupts sequencing, categorization, and task flow, even for lifelong routines. The brain struggles to:
Categorize items correctly (frozen vs. refrigerated)
Remember the steps of a familiar routine (unpack groceries → put frozen items in freezer)
Monitor and correct errors (notice the ice cream is melting)
Why This Matters for Communication
If the brain can't sequence a simple task like putting away groceries, it's also struggling to sequence thoughts in conversation, follow the thread of a discussion, or organize ideas into coherent narratives. Speech therapists see this in discourse-level breakdowns: stories that skip around, conversations that lose the main point, difficulty following multi-turn exchanges.
How Speech Therapy Helps with Sequencing
SLPs specialize in breaking down complex tasks into manageable steps and creating supports to help people successfully complete them:
Visual schedules with pictures
Step-by-step written instructions
Color-coded organizational systems
Verbal routines that provide structure ("First we do this, then we do that")
These same strategies support both practical daily tasks and communication success.
🧠 Anecdote Spotlight: Overfeeding the Dog
One caregiver noticed their loved one fed the dog multiple times throughout the day, forgetting they'd already done it. The dog was gaining weight, and eventually the family realized their loved one genuinely couldn't remember whether or not they'd fed the pet.
Source: https://www.reddit.com/r/AskReddit/comments/1owiser/comment/norvgse/
Clinical Insight
This often shows both memory loss and loss of situational awareness. The person can't remember the recent past, and they've also lost the ability to use contextual clues to figure it out (empty food bowl vs. full food bowl, dog acting hungry vs. disinterested).
The Dangerous Parallel
If this is happening with pet care, it's likely happening with medication, meals, and other important daily routines. This is when safety becomes a critical concern.
🧠 Anecdote Spotlight: Giving Away All Their Money
One early sign of dementia is giving away things, especially things that held some personal meaning and were kept for years. In some cases, it’s money that’s being given away. This next anecdote starts off as a conversation about mounting bills between a mother and their child, but a quick look into things reveals that all those “bills” were really just requests from charity, and mom kept on giving and giving, feeling like she was paying off a debt more than making a conscious contribution.
Source: https://www.reddit.com/r/AskReddit/comments/1owiser/comment/nouehwc/
Clinical Insight
Judgment declines early in dementia, especially around finances, scams, and persuasive communication. The frontal lobes, which help us evaluate situations critically, anticipate consequences, and resist manipulation, begin to fail. People become vulnerable to:
Scams and fraud
High-pressure sales tactics
Emotional manipulation
Poor financial decisions
The Communication Vulnerability
This is particularly concerning from a communication standpoint because people with declining judgment often can't recognize when they're being deceived through language. They take statements at face value, miss sarcasm or deception, and struggle to evaluate the credibility of information.
Protective Strategies
While speech therapy can't prevent financial exploitation directly, we can:
Work with families on communication strategies that help the person feel respected while maintaining safety
Teach caregivers how to redirect without triggering defensiveness
Help the person understand and use structured decision-making supports
Facilitate difficult family conversations about safety and autonomy
PART 4: Speech & Communication Changes
Now we come to the heart of what speech-language pathologists specialize in: direct changes to language, speech, and communication.
These changes often appear before major memory decline becomes obvious to others. Families sense that conversations feel different, but they can't always pinpoint why. This is where the expertise of a speech therapist becomes invaluable.
🧠 Anecdote Spotlight: Subtle Speech Changes
A family noticed their loved one had slight alterations in the way they spoke…not slurring or mispronouncing, just...different. The rhythm was off, the cadence had changed, or there was something indefinable about their speech that didn't sound quite like them anymore.
Source: https://www.reddit.com/r/AskReddit/comments/1owiser/comment/nor88s0/
Clinical Insight
Alzheimer's disease and other dementias can disrupt multiple aspects of speech production and language formulation:
Word-finding (searching for the right word)
Phrasing and sentence structure
Speech rhythm and cadence (prosody)
Articulation clarity
Voice quality
These changes often precede obvious cognitive decline because the language centers of the brain are affected early.
What a Speech Therapist Assesses
A comprehensive speech-language evaluation can identify:
Subtle word-finding difficulties (anomia)
Reduced syntactic complexity (simpler sentence structures)
Changes in speech rate or fluency
Difficulty with abstract language
Problems with narrative organization
Decreased use of specific vocabulary
Why Early Assessment Matters
Catching these changes early allows us to:
Establish baseline abilities before further decline
Introduce compensatory strategies while the person can still learn new techniques
Support maintained communication for as long as possible
Reduce frustration for both the person with dementia and their family
🧠 Anecdote Spotlight: Simpler Conversations
Someone who once held complex, nuanced discussions about politics, literature, or philosophy began speaking in shorter, simpler sentences. Their contributions to conversation became more basic, their observations less sophisticated.
Source: https://www.reddit.com/r/AskReddit/comments/1owiser/comment/nouqdwf/
Clinical Insight
Cognitive load directly affects language complexity. As cognitive processing declines, speech naturally simplifies because:
The brain has fewer resources for complex sentence construction
Working memory can't hold long, multi-clause sentences
Abstract thinking becomes more difficult
The mental effort of conversation increases
This isn't a conscious choice. It's the brain adapting to its reduced capacity.
How Speech Therapy Supports This
A speech-language pathologist can:
Assess which level of language complexity remains accessible
Teach family members to match their communication style to the person's current abilities
Provide strategies for maintaining meaningful conversation despite simplification
Help families grieve the loss of intellectual exchange while finding new ways to connect
Introduce supported conversation techniques that scaffold complex ideas
The Family Communication Training Component
One of the most valuable things a speech therapist can do is teach family members how to communicate in ways that:
Don't talk down to the person
Support understanding without overwhelming
Maintain dignity and respect
Allow for genuine connection despite cognitive changes
This training prevents the common pattern where families either over-simplify (talking to adults like children) or continue with complex communication that leaves the person lost and frustrated.
🧠 Anecdote Spotlight: Repetitive Phrases
A loved one began repeating the same phrases, stories, or even sing-song expressions constantly. In this instance, a grandmother began to have a catch-phrase they repeated whenever someone said, “Goodnight,” or, “fair enough.”
Source: https://www.reddit.com/r/AskReddit/comments/1owiser/comment/nouxxlu/
Clinical Insight
Repetition serves several functions for a brain affected by dementia:
It's soothing and reduces anxiety when new content is hard to generate
It reflects perseveration: the brain getting "stuck" on an idea or phrase
It may be an attempt to maintain conversation when novel language is difficult
It can be an expression of an unmet need (the repeated content may have meaning)
What This Looks Like in Daily Life
Families often describe:
The same question asked over and over ("What time is dinner?" "Where's Mom?" "Did I take my pills?")
The same story told repeatedly, sometimes with variations
Favorite phrases or expressions repeated throughout conversation
Getting stuck on a particular topic or theme
Speech Therapy Interventions for Repetition
An SLP can help by:
Identifying whether repetition signals an unmet need that can be addressed
Teaching redirection techniques that don't dismiss or shame the person
Creating communication supports that answer repeated questions visually
Developing topics and activities that engage the person beyond the repeated content
Training families in validation techniques that acknowledge the communication attempt
A Note on Validation
One powerful approach is validation therapy, or acknowledging the emotion or need behind the repetition rather than correcting the behavior. For example:
Instead of: "You just asked me that! I told you dinner is at 6:00!" Try: "You're thinking about dinner. That must mean you're getting hungry. Dinner will be ready soon, and I'm making your favorite."
What We’ve Covered So Far and What's Coming in Part 2
If you've made it this far, you've read real family stories about the subtle, surprising ways dementia first appears. You've learned that:
✓ Memory loss often isn't the first sign: Behavior changes, communication shifts, and judgment problems frequently appear first
✓ Communication is central to nearly every early symptom, which is why speech-language pathologists play such a crucial role in early detection and intervention
✓ Small changes matter: The "little things" families initially dismiss often turn out to be significant warning signs
✓ Masking is common: People with early dementia can hide their struggles remarkably well, especially in brief social interactions
✓ Every person's experience is different, but patterns emerge that can help families recognize when something deserves professional attention
Coming in Part 2
In the second part of this series, you'll find:
📌 More family stories covering:
Sensory changes (taste, smell, perception)
Emotional and psychological shifts
Sleep and daily rhythm changes
Movement, falls, and physical red flags
Eating, alcohol use, and self-care changes
Confabulation (telling impossible stories)
Signs specific to non-Alzheimer's dementias
📋 A comprehensive, printable checklist of early warning signs organized by category
🏠 Detailed guidance on how in-home speech therapy can help at each stage of cognitive decline
💡 Practical next steps, including:
When and how to seek evaluation
What to expect from speech therapy
Communication strategies families can start using immediately
Resources and support for the journey ahead
Don't Wait: Recognize the Signs and Take Action
If you've recognized your loved one in any of these stories, please don't wait to read Part 2. The information there could make a critical difference in:
How soon you seek help
What kind of support you access
How well you're able to maintain communication and connection
Your loved one's quality of life going forward
What You Can Do Right Now
While you're waiting to read Part 2, here are three important steps:
1. Start Documenting What You Notice
Keep notes on your phone or in a journal:
Date and time of concerning incidents
What specifically happened
How often similar things occur
Your loved one's reaction
This documentation will be invaluable when you seek professional evaluation.
2. Trust Your Instincts
If something feels "off," it probably is. Family members who spend significant time with a person are often the first to notice subtle changes that others miss. Don't dismiss your concerns just because:
The person seems fine in public
A doctor said "everything's normal" after a brief visit
Other family members haven't noticed anything
You're worried about overreacting
Early intervention makes a significant difference. It's always better to evaluate and find out you're being cautious than to wait and miss the window for effective support.
3. Consider Speech-Language Evaluation
If you've noticed communication changes, even subtle ones, consider seeking evaluation from a speech-language pathologist who specializes in cognitive-communication disorders. You don't need to wait for a dementia diagnosis or a doctor's referral to connect with a speech therapist.
Early speech-language assessment can:
Identify subtle changes that warrant further evaluation
Establish baseline abilities before further decline
Provide family training in effective communication strategies
Introduce memory supports and compensatory techniques
Ensure swallowing safety
Nina Minervini provides comprehensive in-home speech therapy sessions for adults with cognitive-communication concerns in the areas surrounding Lake Worth, Boynton Beach, and Delray Beach. Working in your home allows for real-world assessment of how cognitive changes affect daily communication and function.
📞 To learn more or schedule a consultation:
Phone: (561) 797-2343
Email: ninaminervini11@gmail.com
Website: www.speechpalmbeach.com
The Most Important Thing to Remember
Dementia doesn't have to be a journey you face alone. Early recognition, professional support, and effective communication strategies can make an enormous difference in quality of life for both the person with cognitive changes and their family.
The stories you've read here are from families who looked back and said, "I wish we'd known sooner." You have the advantage of learning from their experiences.
Don't wait for a crisis. Act on what you're noticing now. Get the finest in-home senior care in South Florida.
Continue to Part 2
Ready to learn more? The Subtle, Surprising Early Signs of Dementia Part 2 includes:
Additional family stories covering sensory changes, emotional shifts, sleep problems, and more
A comprehensive early warning signs checklist you can print and use
Detailed information about how in-home speech therapy can help at each stage
Clear next steps for getting the support your family needs
Resources for navigating this journey with professional guidance
The second half of this series includes even more stories and provides the practical tools and professional guidance that can transform how your family experiences this challenging journey.