Swallowing Evaluation and Therapy in Lake Worth, FL
Eating and drinking should be safe, enjoyable parts of daily life, not a source of stress, fear, or physical danger. If you or someone you love coughs or chokes when eating, feels food getting stuck in the throat, avoids certain textures or foods entirely, takes an unusually long time to finish meals, or has experienced unexplained weight loss, you may be dealing with dysphagia, a medical term for swallowing difficulty.
At Palm Beach Speech Therapy, licensed speech-language pathologist Nina Minervini, M.S., CCC-SLP provides comprehensive in-home swallowing evaluation and therapy throughout Lake Worth, Florida, helping adults and seniors eat and drink safely again while restoring comfort, dignity, and confidence at the table.
Evidence-Based Parkinson’s Rehabilitation
For clients seeking a structured, research-supported plan, Nina provides a Parkinson’s voice, cognition, and swallowing rehabilitation program that integrates SPEAK OUT!®, swallowing therapy, and cognitive-communication treatment.
Contact: Swallowing Evaluation & Therapy in Lake Worth
Complete this quick form and Nina will contact you within 24 hours to discuss your needs.
Understanding Dysphagia: More Than Just "Difficulty Swallowing"
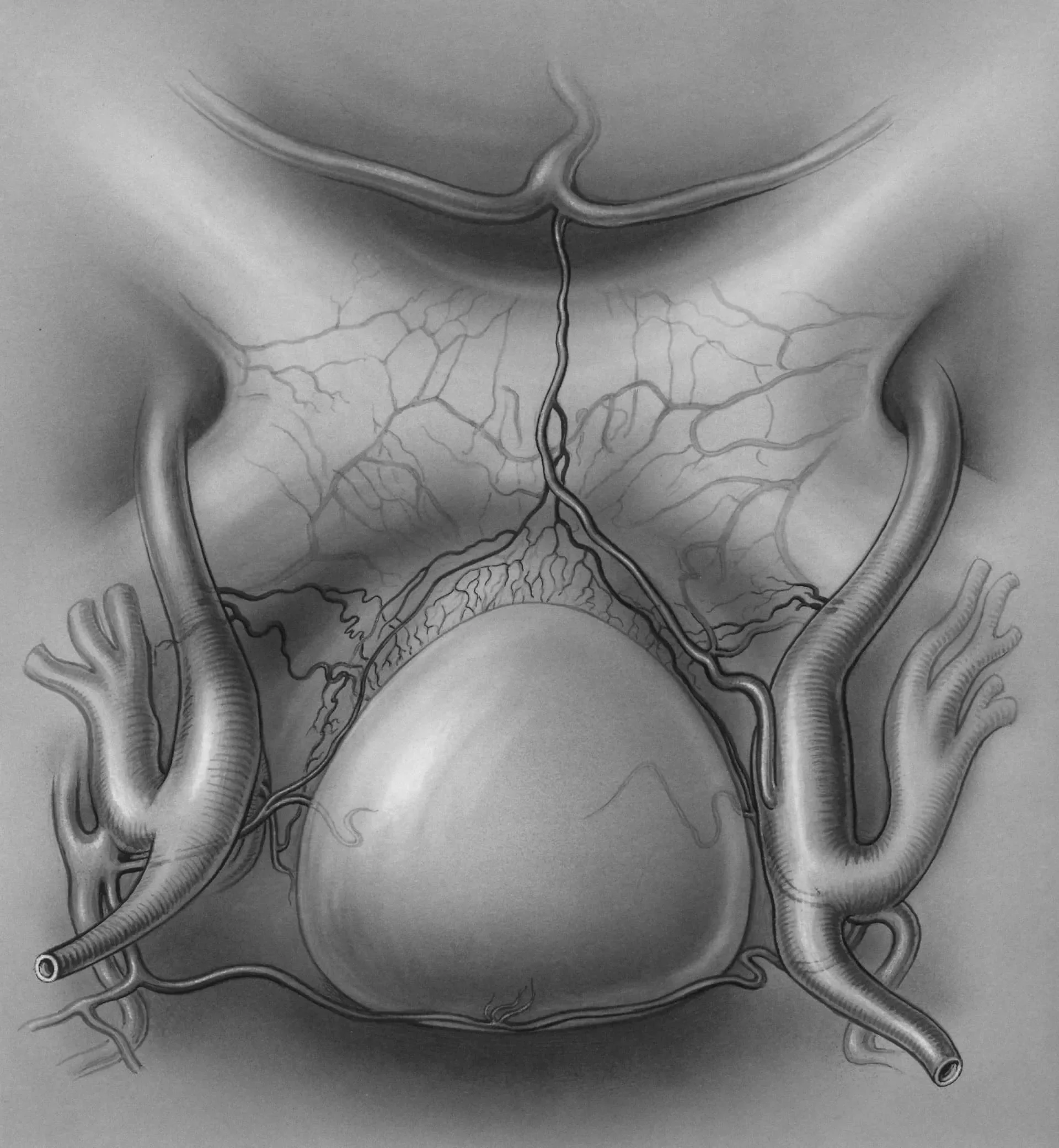
Swallowing is one of the most complex processes the human body performs, and it’s one we rarely think about until something goes wrong. Each swallow involves the precise coordination of over 50 pairs of muscles across the mouth, throat, esophagus, and airway, all working together in less than one second.
When illness, injury, aging, or neurological changes disrupt this coordination, dysphagia can develop. Food or liquid may not move safely and efficiently from the mouth to the stomach. Instead, it may:
Get stuck in the throat or esophagus
Enter the airway (called aspiration), causing coughing, choking, or silent aspiration
Take excessive time or effort to swallow
Cause pain, discomfort, or a sensation of a lump in the throat
Lead to avoidance of eating, resulting in malnutrition, dehydration, and weight loss
The most serious risk of untreated dysphagia is aspiration pneumonia, a lung infection caused when food, liquid, or saliva enters the lungs. Aspiration pneumonia is a leading cause of hospitalization and mortality in older adults and individuals with neurological conditions.
Common Causes of Swallowing Difficulty in Lake Worth
Dysphagia can result from a wide range of medical conditions and life events. Understanding the underlying cause is essential to creating an effective treatment plan.
Neurological Causes
Stroke or transient ischemic attack (TIA) — the most common cause of sudden-onset dysphagia
Parkinson's disease — progressive weakness and reduced coordination
Amyotrophic lateral sclerosis (ALS) — muscle weakness affecting swallowing and speech
Multiple sclerosis (MS) — demyelination affecting nerve signals
Dementia and Alzheimer's disease — cognitive decline impacting the ability to initiate or complete swallowing
Traumatic brain injury (TBI) — damage to areas controlling swallowing reflexes
Cerebral palsy — motor control challenges affecting oral and pharyngeal function
Structural and Medical Causes
Head and neck cancer — tumors that obstruct or alter swallowing anatomy
Radiation therapy — fibrosis, reduced saliva production, and tissue damage
Esophageal disorders — strictures, reflux, or motility problems
Post-surgical changes — after intubation, tracheostomy, or oral/throat surgery
Zenker's diverticulum — a pouch in the esophagus that traps food
Age-Related Causes
Sarcopenia — natural muscle loss and weakness with aging
Reduced saliva production — dry mouth affecting bolus formation
Slower reflexes — delayed swallow initiation or airway closure
Medication side effects — dry mouth, drowsiness, or muscle relaxation
Warning Signs: When to Seek an In-Home Swallowing Evaluation
Many people live with swallowing difficulty for months or even years before seeking help, often because symptoms develop gradually or are mistaken for normal aging. Recognizing the signs early can prevent serious complications and improve outcomes.
Contact Palm Beach Speech Therapy in Lake Worth if you or a loved one experiences:
Coughing or choking during or after eating or drinking
A wet, gurgly, or hoarse voice after swallowing
Feeling like food is stuck in the throat or chest
Needing to swallow multiple times to clear food
Avoiding certain foods or textures (especially meats, breads, or thin liquids)
Taking longer than 30 minutes to finish a meal
Unintentional weight loss or dehydration
Frequent throat clearing or a need to cough after swallowing
Recurrent pneumonia or respiratory infections
Shortness of breath during meals
Drooling or difficulty managing saliva
Pain when swallowing (odynophagia)
Fear or anxiety around eating
Who Benefits from Swallowing Therapy?
Swallowing therapy is appropriate for adults and seniors experiencing dysphagia related to:
Stroke recovery (acute and chronic)
Parkinson's disease and Parkinsonism
ALS, MS, and other neurodegenerative diseases
Post-cancer treatment (radiation, surgery, chemotherapy)
Dementia and cognitive decline
Traumatic brain injury
Post-surgical recovery (oral, throat, esophageal, cardiac)
Prolonged intubation or tracheostomy
Age-related swallowing changes (presbyphagia)
Esophageal dysmotility or reflux
Progressive supranuclear palsy (PSP) or other rare neurological conditions
Whether your swallowing difficulty appeared suddenly or developed gradually over time, Nina has the expertise to evaluate your needs and design a therapy plan that works.
Comprehensive Swallowing Evaluation: What to Expect
Nina conducts thorough, individualized swallowing evaluations in the comfort and privacy of your Lake Worth home. The clinical swallow evaluation (CSE) is the foundation of safe, effective dysphagia treatment.
Step 1: Medical and Case History Review
The evaluation begins with a detailed conversation about:
Medical diagnoses and recent hospitalizations
Onset and progression of swallowing symptoms
Current diet, hydration, and eating habits
Medications that may affect swallowing
Previous swallowing studies or therapies
Respiratory health and history of pneumonia
Weight changes and nutritional status
Caregiver observations and mealtime concerns
Step 2: Oral-Motor and Sensory Examination
Nina assesses the structures and functions involved in swallowing:
Lip, tongue, jaw, and cheek strength and range of motion
Soft palate elevation and gag reflex
Oral sensation and awareness
Dentition and oral hygiene
Voice quality and clarity
Cough strength and airway protection reflexes
Step 3: Swallowing Trials with Food and Liquid
Using real foods and beverages, Nina observes how you swallow different:
Textures — puree, minced, soft, or regular solid foods
Liquid consistencies — thin, nectar-thick, honey-thick, or pudding-thick liquids
Portion sizes — teaspoon, tablespoon, cup, or self-selected amounts
She watches for signs of swallowing difficulty, including:
Delayed swallow initiation
Coughing or choking
Wet vocal quality after swallowing
Residue remaining in the mouth or throat
Multiple swallows per bite
Effortful or painful swallowing
Step 4: Risk Assessment and Safety Recommendations
Based on the clinical findings, Nina identifies:
Aspiration risk (silent or overt)
Safe vs. unsafe foods and liquids
Need for diet texture modifications
Positioning or compensatory strategies
Whether an instrumental swallow study is warranted
Step 5: Customized Treatment Plan
You'll leave the evaluation with:
A clear understanding of your swallowing function
Immediate safety recommendations for meals
A personalized therapy plan with measurable goals
Caregiver education and printed resources
Coordination with your physician or medical team as needed
Instrumental Swallow Studies: When Imaging Is Needed
In some cases, a clinical swallow evaluation alone cannot fully visualize what's happening during the swallow. Nina may recommend an instrumental swallow study to obtain objective, detailed information about swallowing physiology.
Modified Barium Swallow Study (MBS/MBSS)
Also called a videofluoroscopic swallow study (VFSS), this is the gold standard for dysphagia assessment. During the study:
You swallow foods and liquids mixed with barium (a safe contrast agent)
Real-time X-ray imaging captures the entire swallow process
Nina and a radiologist observe timing, coordination, and aspiration
Therapeutic strategies are tested during the study to determine what works best
The MBS is performed at an outpatient radiology center. Nina coordinates scheduling and often attends the study to ensure continuity of care.
Fiberoptic Endoscopic Evaluation of Swallowing (FEES)
This procedure uses a thin, flexible scope passed through the nose to view the throat and vocal cords during swallowing. FEES:
Does not use radiation
Can be performed at bedside or in a clinic
Allows direct visualization of secretions, residue, and aspiration
Provides real-time feedback on compensatory strategies
Nina collaborates with ENT physicians or FEES-certified clinicians to arrange this study when appropriate.
Swallowing Therapy: Retraining the Body to Eat Safely
Once your swallowing evaluation is complete, therapy begins. The goal is to restore safe, functional swallowing, not just manage symptoms, but address the root causes of dysphagia whenever possible.
Therapy is conducted one-on-one in your Lake Worth home, using real foods, your own dishes, and your typical mealtime routines. This real-world approach ensures skills transfer directly to daily life.
Swallowing Exercises (Therapeutic Interventions)
Evidence-based exercises target the specific muscles and movements needed for safe swallowing:
Thermal-tactile stimulation — a cold sensory cue that jump-starts the swallow reflex
Mendelsohn maneuver — prolongs laryngeal elevation to improve airway closure
Supraglottic swallow — strengthens voluntary airway protection
Effortful swallow — increases tongue base retraction to clear residue
Shaker exercise — strengthens muscles that open the upper esophageal sphincter
Masako maneuver — improves pharyngeal contraction
Tongue strengthening exercises — using resistance tools or the IOPI device
Chin tuck against resistance (CTAR) — builds suprahyoid muscle strength
Vocal fold adduction exercises — improves airway closure and reduces aspiration
Exercises are prescribed based on your specific impairments, practiced during therapy sessions, and assigned as home practice for maximum benefit.
Compensatory Strategies
These techniques change how you swallow to make eating safer immediately, without requiring muscle strengthening:
Chin tuck — narrows the airway entrance to reduce aspiration risk
Head rotation — directs food away from a weaker side
Head tilt — uses gravity to guide the bolus
Effortful or double swallow — clears residue more completely
Smaller bites and slower pace — reduces overload and improves coordination
Alternating solids and liquids — clears residue and improves efficiency
There are also a growing number of mindfulness exercises for swallowing that can help assist with swallowing function in adults, which we can practice during sessions.
Diet Texture and Liquid Consistency Modifications
When certain textures or thin liquids are unsafe, Nina provides clear guidance on:
International Dysphagia Diet Standardisation Initiative (IDDSI) levels for food and liquid
Safe food preparation and recipe modifications
How to thicken liquids to the appropriate consistency
How to progress toward less restrictive textures as swallowing improves
Diet modifications are always temporary whenever possible. The goal is to return to a normal diet as soon as it's safe to do so.
Caregiver and Family Training
Family members and caregivers play a critical role in dysphagia management. Nina provides training on:
How to position the person for safe swallowing
Recognizing signs of aspiration or distress
Safe feeding techniques and pacing
How to prepare modified textures and thickened liquids
What to do in an emergency (choking, aspiration)
How to encourage eating without causing anxiety or frustration
Empowering caregivers creates a safer, more supportive mealtime environment.
Ongoing Reassessment and Progression
Swallowing therapy is dynamic. Nina continuously monitors your progress and adjusts the treatment plan based on:
Improvements in strength, coordination, and safety
Changes in medical status or medications
Tolerance of upgraded textures or consistencies
Achievement of functional eating goals
Caregiver feedback and observations
The ultimate goal is always to restore the most normal, least restrictive diet possible while maintaining safety and quality of life.
Evidence-Based Care Grounded in Research
Every treatment plan is built on current research and clinical best practices. Nina uses evidence-based protocols endorsed by the American Speech-Language-Hearing Association (ASHA), peer-reviewed dysphagia literature, and clinical guidelines from leading medical institutions.
Evidence-based care means:
Your therapy is proven to work, not based on tradition or guesswork
Goals are measurable, specific, and achievable
Outcomes are tracked and documented
Treatment evolves with emerging research and your individual progress
You can trust that your swallowing therapy is grounded in science and designed to deliver real, lasting results.
Why Swallowing Therapy Matters: The Impact of Untreated Dysphagia
Dysphagia is a serious medical condition with life-altering consequences when left untreated.
Physical Health Risks:
Aspiration pneumonia (a leading cause of death in older adults)
Malnutrition and unintended weight loss
Dehydration and electrolyte imbalances
Increased hospitalizations and medical costs
Reduced immune function and wound healing
Decline in overall health and functional independence
Emotional and Social Impact:
Fear and anxiety around eating
Social isolation and withdrawal from family meals or dining out
Depression and reduced quality of life
Loss of independence and dignity
Caregiver stress and burnout
With effective therapy, you can:
Eat and drink safely without fear of choking
Maintain proper nutrition and hydration
Prevent aspiration pneumonia and hospitalizations
Enjoy meals with family and friends again
Regain independence and confidence
Improve overall health and longevity
Relearning to swallow safely is more than a physical skill, and it's a path back to independence, joy, dignity, and a better quality of life.
The Benefits of In-Home Swallowing Therapy
Receiving dysphagia care in your Lake Worth home offers significant advantages:
Real-world practice — therapy happens with your own foods, utensils, and routines
Comfort and convenience — no stressful transportation or clinic waiting rooms
Caregiver involvement — family members can participate and learn
Privacy and dignity — eating challenges are addressed in a safe, familiar space
Better outcomes — skills learned at home transfer more easily to daily life
Flexible scheduling — sessions fit your routine and energy levels
Proudly Serving Lake Worth and Surrounding Communities
Palm Beach Speech Therapy provides in-home swallowing evaluation and therapy throughout Lake Worth Beach and neighboring areas, including:
South Palm Park
Bryant Park
Parrot Cove
College Park
Mango Groves
Eden Place
Sunset Ridge
Old Lucerne
Downtown Jewel
Lake Osborne
Lucerne Pointe
Many clients enjoy the comfort of receiving therapy in their own homes, whether in a quiet neighborhood near Bryant Park, along Palmway, overlooking the Intracoastal Waterway, or in one of Lake Worth's vibrant senior living communities. In-home care eliminates transportation challenges, reduces anxiety, and allows therapy to happen in the real-world environment where eating actually occurs.
Start Improving Your Quality of Life Today
You don't have to live with the fear, frustration, and isolation of swallowing difficulty. Help is available, and it starts with a single phone call.
Schedule a swallowing evaluation in Lake Worth by calling (561) 797-2343 or by completing the contact form. Nina will respond personally within 24 hours to discuss your concerns, answer your questions, and schedule your first appointment.
Take the first step toward eating safely, confidently, and joyfully again.
Frequently Asked Questions | Swallowing (Dysphagia) Care in Lake Worth
How do I know if I need a swallowing evaluation?
If you cough or choke with meals, feel food “sticking,” need multiple swallows, avoid certain textures, or have unexplained weight loss or recurrent chest infections, an evaluation is appropriate. If breathing is compromised or choking is severe, call 911 immediately.
How long does a swallowing evaluation take?
Initial in-home evaluations typically take 60–90 minutes, including history, oral-motor exam, swallowing trials, risk screening, and same-day safety recommendations.
Do you offer in-home swallowing therapy in Lake Worth?
Yes. Palm Beach Speech Therapy provides in-home evaluation and treatment throughout Lake Worth Beach and nearby areas (e.g., South Palm Park, Bryant Park, Parrot Cove, College Park, Mango Groves, Lake Osborne).
Will I need to change my diet permanently?
Not necessarily. Diet texture or liquid-thickening changes are often temporary safety measures while therapy strengthens and retrains the swallow. When it’s safe, we work toward the least restrictive diet.
What happens during therapy?
Therapy is individualized and may include evidence-based exercises (e.g., effortful swallow, Mendelsohn, CTAR), compensatory strategies (chin tuck, head turn, pacing), and IDDSI-guided diet coaching, plus caregiver training.
Do you coordinate instrumental studies like MBSS or FEES?
Yes. When indicated, we coordinate a Modified Barium Swallow Study (MBSS) or FEES with local partners and integrate results into your plan of care.
Can long-standing dysphagia still improve?
Often, yes. Even chronic swallowing difficulty can benefit from targeted exercises, strategy training, and gradual diet advancement when appropriate.
Is swallowing therapy covered by insurance?
Many plans, including Medicare, cover medically necessary speech therapy for dysphagia. We provide documentation and can guide you on next steps with your plan. Private-pay options are available.
What should I have ready for my evaluation?
Recent medical notes (if available), a medication list, and small portions of typical foods and liquids (including any you find difficult). A caregiver’s observations are very helpful.
How soon will I notice improvements?
Some people notice safer, easier meals after their first visit with strategy changes; strengthening and endurance gains typically emerge over weeks with consistent practice.
Do you help caregivers?
Absolutely. We train family and caregivers on safe feeding, positioning, pacing, recognizing signs of aspiration, and how to prepare IDDSI-appropriate foods and liquids.
Is there an age limit for swallowing therapy?
No. Adults of all ages in Lake Worth recovering from stroke, neurodegenerative conditions, cancer recovery, or age-related changes can benefit from dysphagia therapy.
Let’s Tackle Swallowing Difficulties Together
Start having more confident meals, enjoy your time at the table, and get the proper nutrition you need as safely as possible with speech therapy sessions in Lake Worth. Nina comes to your home.