The 1-Minute Cognitive-Communication Screening Every Physician Should Use in Post-Stroke and Parkinson's Care
The Hidden Epidemic in Neurological Follow-Up Care
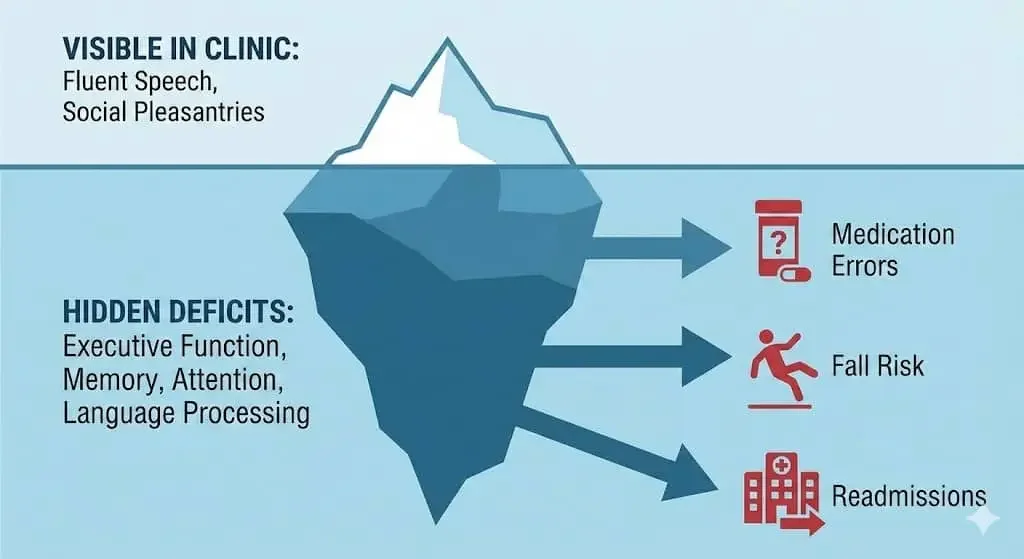
Every day, patients walk out of neurology appointments with undetected cognitive-communication deficits that will quietly derail their recovery.
They sound coherent during brief clinical exchanges.
They answer yes-or-no questions appropriately.
Their speech is fluent enough that nothing raises immediate concern.
Yet within weeks, these same patients will miss critical medication doses, make unsafe decisions, experience preventable falls, or end up back in the emergency department, all because subtle impairments in attention, memory, executive function, or language processing went unidentified during routine follow-ups.
Cognitive-communication impairments represent one of the most under-recognized yet devastating consequences of stroke and Parkinson's disease. The consequences extend far beyond the examination room: medication errors, treatment non-adherence, social isolation, caregiver burnout, hospital readmissions, and loss of independence all trace back to deficits that could have been caught with a 60-second screening.
The Scope of the Problem: What Research Reveals
The prevalence of post-stroke cognitive impairment is staggering. According to research published in Stroke by Cramer and colleagues, between 20% and 60% of stroke survivors experience persistent cognitive deficits in domains including attention, memory, and executive function, all deficits that persist well beyond the acute recovery phase and often remain unaddressed in standard care protocols.
What makes these impairments particularly insidious is their subtlety. A comprehensive analysis in Stroke Prevention and Treatment demonstrates that substantial chronic cognitive-communication impairment frequently occurs even in patients without obvious aphasia. These individuals may pass casual conversation tests while harboring significant deficits in complex language processing, reasoning, and functional communication.
The relationship between executive dysfunction and communication breakdown is particularly well-documented. Research by Schumacher and colleagues in Frontiers in Neurology reveals the deeply intertwined nature of executive function deficits and language impairments in post-stroke aphasia, showing that these domains cannot be treated as separate entities.
Similarly, work by Yao and colleagues demonstrates the high prevalence of non-linguistic cognitive deficits in aphasia populations, underscoring that language testing alone misses critical functional impairments.
In Parkinson's disease, executive dysfunction emerges as an equally pervasive problem, quietly undermining patients' capacity to organize daily routines, follow complex treatment regimens, and maintain safety awareness, often while motor symptoms receive the bulk of clinical attention.
Why Traditional Follow-Ups Miss These Deficits
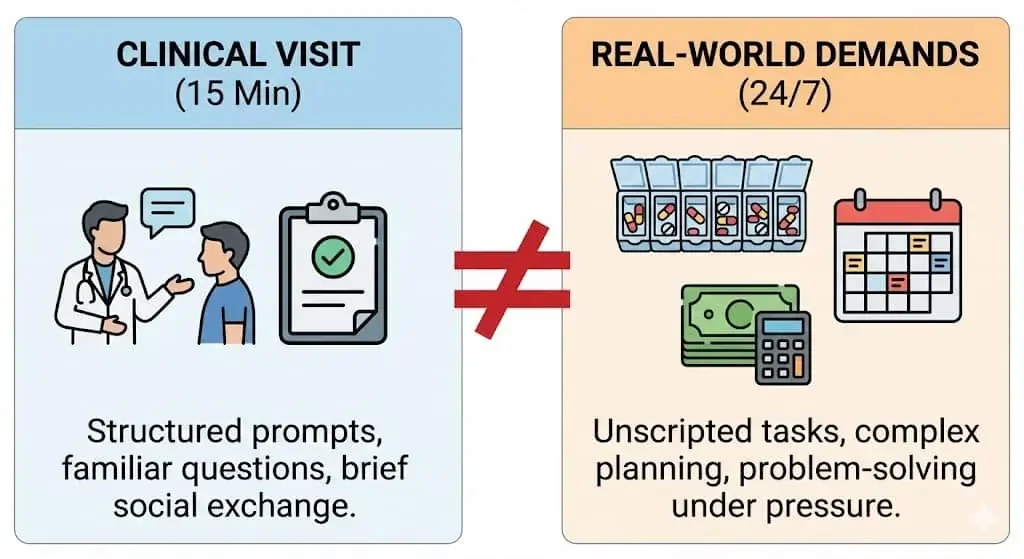
Standard neurological follow-up appointments are designed to be efficient, focused encounters.
In a 15-minute visit, physicians must review medications, assess motor function, screen for complications, address acute concerns, and document meticulously.
The conversational demands of this interaction (answering direct questions, responding to familiar prompts, engaging in social pleasantries) rarely challenge the specific cognitive-communication skills that govern real-world function.
Patients with significant impairments may:
Answer "yes" when asked if they understand their medication schedule, while being unable to independently execute that schedule at home
Appear engaged during the visit while missing crucial nuances in treatment discussions
Compensate effectively in structured clinical conversations while struggling dramatically with unscripted daily communication
Mask word-finding difficulties through circumlocution and vague language that sounds appropriate in the moment
Family members often notice problems months before clinical teams do, but may not recognize these changes as treatable neurological symptoms or may hesitate to raise concerns during brief appointments.
The Clinical Impact of Unidentified Cognitive-Communication Impairments
The consequences of missed cognitive-communication deficits ripple across every aspect of patient care and recovery:
Medication Safety: Patients with working memory deficits or impaired sequencing abilities struggle to manage complex medication regimens, leading to missed doses, incorrect timing, dangerous drug interactions, and preventable complications.
Treatment Adherence: When patients cannot fully process discharge instructions, comprehend follow-up appointment details, or remember rehabilitation protocols, even excellent treatment plans fail.
Fall Risk: Cognitive-communication impairments affect safety awareness, judgment, problem-solving under pressure, and the ability to follow safety precautions (all factors that directly increase fall risk independent of motor deficits).
Healthcare Utilization: Preventable emergency department visits and hospital readmissions frequently stem from cognitive-communication breakdowns that interfere with self-management, early symptom recognition, and appropriate help-seeking.
Social Withdrawal and Depression: Patients who struggle with communication demands often withdraw from social engagement, leading to isolation, depression, and reduced quality of life, even when physical recovery progresses well.
Caregiver Burden: Family members who don't understand the cognitive-communication basis of concerning behaviors may misinterpret them as willfulness, laziness, or personality change, leading to conflict, guilt, and burnout.
Each of these outcomes is potentially preventable through early identification and appropriate speech-language pathology intervention.
The Solution: A 1-Minute Red-Flag Screening Tool
The good news is that physicians don't need specialized training or lengthy assessment protocols to identify patients at risk. A brief, observation-based screening can be seamlessly integrated into routine follow-up visits and dramatically improve detection rates.
When to Use This Screening
Implement this red-flag checklist during any routine follow-up with patients who have:
Stroke (ischemic or hemorrhagic, at any time post-onset)
Transient ischemic attack (TIA)
Parkinson's disease or Parkinsonism
Dementia or mild cognitive impairment
Brain tumor or neurosurgical history
The screening requires no special materials, no scoring sheets, and no additional time beyond the normal clinical conversation. Simply observe and note any red flags during your standard interaction with the patient.
The Red-Flag Checklist
Communication & Language Processing Red Flags
❗ Difficulty following multi-step instructions: Patient struggles when you explain medication changes, rehabilitation protocols, or follow-up procedures that involve multiple sequential steps
❗ Word-finding difficulties: Noticeable pauses mid-sentence, talking around words they can't retrieve, using vague terms ("thing," "stuff") or excessive circumlocution to compensate for missing specific vocabulary
❗ Trouble with complex information: Visible confusion or inability to process explanations involving conditional logic, risk-benefit discussions, comparison of treatment options, or abstract medical concepts
❗ Repetitive questions or comments: Asking the same question multiple times within a single visit despite receiving clear answers
❗ Inconsistent responses: Providing contradictory information when asked the same question in different ways
Executive Function Red Flags
❗ Medication or appointment management breakdown: New or worsening inability to manage pill organizers, remember to take medications, track refills, or keep track of appointment schedules
❗ Impaired sequencing and organization: Missing steps in familiar routines, mixing up the order of instructions, difficulty planning even simple multi-step tasks
❗ Financial or household management deterioration: Previously independent patients now struggling with bills, checkbook management, grocery planning, or maintaining home routines
❗ Poor judgment or safety awareness: Making risky decisions without apparent recognition of danger, such as attempting unsafe transfers, refusing needed assistance, or making impulsive choices that contradict medical advice
❗ Difficulty with task initiation or completion: Starting activities but unable to carry them through, or profound difficulty getting started on necessary tasks
Behavioral, Cognitive, & Social Red Flags
❗ Family reports of personality or behavioral changes: Loved ones describe increased impulsivity, frustration intolerance, emotional lability, apathy, or social withdrawal that represents a change from baseline
❗ Irritability or confusion during routine conversation: Patient becomes frustrated, defensive, or confused during straightforward clinical discussions that shouldn't provoke these reactions
❗ Processing speed concerns: Marked slowing in responding to questions, difficulty keeping up with normal conversational pace, appearing overwhelmed by routine interactions
❗ Mental fatigue: Rapid cognitive decline over the course of a visit, with patient becoming noticeably less engaged, coherent, or responsive after 10-15 minutes
❗ Social withdrawal or isolation: Patient or family reports decreased participation in previously enjoyed activities, avoiding social situations, or giving up hobbies due to communication or cognitive demands
Interpretation and Action
If you observe even ONE red flag: Consider a speech-language pathology referral for cognitive-communication screening.
If you observe TWO OR MORE red flags: Strongly recommend comprehensive cognitive-communication evaluation by an SLP, and prioritize this referral alongside other post-stroke or neurological care.
If family members raise concerns about any of these areas: Take their observations seriously even if you don't observe problems during the clinical encounter. Family members witness functional performance across diverse, unstructured situations that reveal deficits masked in brief clinical interactions.
What Happens After an SLP Referral?
When you refer a patient for cognitive-communication evaluation, the speech-language pathologist conducts a comprehensive assessment that goes well beyond what can be captured in routine follow-up. This typically includes:
Standardized Cognitive Assessment: Testing across multiple domains including attention and concentration, processing speed, working memory and long-term memory, executive function (planning, organization, problem-solving, cognitive flexibility), reasoning and judgment.
Functional Communication Evaluation: Assessment of real-world communication tasks including following complex spoken and written instructions, comprehending medical information and consent materials, expressing needs and concerns effectively, understanding abstract language and inferences, and managing communication breakdown and repair.
Language Processing Analysis: When indicated, formal evaluation of receptive and expressive language, semantic processing and word retrieval, sentence-level comprehension and formulation, discourse organization and coherence.
Safety and Functional Reasoning: Evaluation of medication management capabilities, safety awareness in daily scenarios, financial management and judgment, ability to recognize and respond to emergencies.
Patient and Family Education: Helping families understand the cognitive-communication basis of observed behaviors, distinguishing neurological symptoms from willful behavior, providing strategies for supporting communication at home.
Treatment Planning: Development of individualized therapy goals targeting specific functional deficits, implementation of compensatory strategies and environmental modifications, coordination with the medical team for unified care planning.
The SLP will communicate findings and recommendations back to you, enabling truly collaborative care that addresses both the medical and functional-cognitive dimensions of neurological recovery.
Why This 60-Second Investment Changes Everything
1. Efficiency Without Compromise
This screening takes less time than explaining medication changes, yet it identifies functional risks that would otherwise emerge as crises weeks or months later.
You're not adding tasks; you're making your existing clinical observations more strategic and purposeful.
2. Prevention of Major Safety Events
The financial and human costs of cognitive-communication-related adverse events are enormous.
A single preventable hospitalization, fall with injury, or medication error costs exponentially more than early SLP intervention, and the human suffering prevented cannot be quantified.
3. Improved Treatment Outcomes Across All Domains
When patients can actually understand, remember, and execute your treatment recommendations, every other intervention you provide becomes more effective.
Physical therapy, occupational therapy, medication management, and lifestyle modifications all depend on intact cognitive-communication skills.
4. Enhanced Patient and Family Satisfaction
Families feel heard and supported when cognitive-communication concerns are acknowledged and addressed proactively rather than dismissed or overlooked.
Patients benefit from validation that their struggles are real, neurologically based, and treatable.
5. Reduced Caregiver Burden and Burnout
When families understand the cognitive-communication basis of challenging behaviors and receive professional support through SLP intervention, caregiver stress decreases significantly and relationships improve.
6. Stronger Interdisciplinary Collaboration
Integrating SLP expertise into routine neurological care creates a true team approach where cognitive-communication function receives the same attention as motor, sensory, and medical management.
Implementation Strategies for Busy Practices
Strategy 1: Build It Into Templates
Add the red-flag checklist to your electronic medical record templates for stroke and Parkinson's follow-up visits as a prompt during documentation.
Strategy 2: Train Medical Assistants
MA staff can be trained to conduct informal observation and flag concerning patterns for physician attention during the visit.
Strategy 3: Create Standing Referral Protocols
Establish automatic SLP consultation for all patients 3-6 months post-stroke or upon Parkinson's diagnosis unless specifically contraindicated.
Strategy 4: Use Family Questionnaires
Provide brief questionnaires to family members in the waiting room asking about functional communication and cognition, which can be quickly reviewed during or after the visit.
Invite a speech-language pathologist to provide brief training to your clinical team on what to listen and watch for during routine encounters.
The Bottom Line: One Minute Can Change a Patient's Trajectory
Cognitive-communication impairments will affect the majority of your stroke and Parkinson's patients at some point in their journey. Most will never receive appropriate evaluation or treatment unless you implement routine screening.
The 1-minute red-flag checklist requires no special equipment, no standardized testing, no additional appointment time. It simply asks you to observe strategically during interactions you're already having and to act on what you observe.
By integrating this screening into every neurological follow-up visit, you ensure that cognitive-communication deficits are identified early, when intervention is most effective, before functional decline accelerates, and while patients and families are still engaged in active rehabilitation.
This simple practice strengthens interdisciplinary care, prevents devastating complications, improves quality of life, and ultimately transforms outcomes for patients navigating the complex challenges of stroke and Parkinson's disease recovery.
Your 60-second screening today could prevent a crisis tomorrow.
Expert Cognitive-Communication Support in Palm Beach County
If you're a physician looking to refer patients for comprehensive cognitive-communication evaluation, or a patient or family member concerned about post-stroke or Parkinson's-related communication and cognitive changes, Palm Beach Speech Therapy provides specialized neurological rehabilitation services throughout Palm Beach County.
Led by Nina Minervini, MS, CCC-SLP, Palm Beach Speech Therapy offers expert evaluation and treatment for the complex cognitive-communication needs of stroke survivors and individuals with Parkinson's disease. Nina's clinical expertise encompasses the full spectrum of post-stroke cognitive rehabilitation, executive function training, functional communication therapy, and evidence-based interventions for the subtle deficits that standard follow-ups often miss.
Specialized Parkinson's Speech and Swallow Program
Nina offers a comprehensive Parkinson's speech and swallow program specifically designed for the unique challenges faced by individuals with Parkinson's disease and Parkinsonism. This specialized program addresses:
Voice projection and speech intelligibility using evidence-based protocols
Swallowing safety evaluation and dysphagia management
Cognitive-communication impairments including executive dysfunction
Functional communication strategies for daily life
Family education and caregiver training
Palm Beach Speech Therapy serves patients throughout Palm Beach County with flexible service options including in-home therapy, teletherapy, and clinic-based sessions to meet the diverse needs of neurological patients and their families.
For physician referrals or to schedule a consultation:
📞 Phone: (561) 797-2343
📧 Email: ninaminervini11@gmail.com
🌐 Online Form: Contact Nina Today
Early identification and intervention transform outcomes. If you or someone you care for is navigating recovery from stroke or living with Parkinson's disease, don't wait for cognitive-communication challenges to become crises. Expert help is available right here in Palm Beach County.