PACE Therapy at Home: 9 Practical Exercises to Support Aphasia Recovery
Living with aphasia can transform everyday conversations into complex challenges. Your thoughts remain clear, but the pathway to sharing them becomes blocked or altered.
This is where PACE therapy emerges as a beacon of hope. It’s a revolutionary approach that recognizes communication extends far beyond spoken words, and you can practice PACE outside of speech therapy sessions with friends and family at home.
By embracing multiple channels of expression and focusing on successful message delivery rather than perfect speech, PACE therapy opens new doors to meaningful connection and interaction.
Table of Contents
Jump to a section below, or scroll to read in full.
- Understanding PACE Therapy
- Who Can Benefit from PACE at Home?
- The Science Behind PACE
- Setting Up Your Home PACE Practice
- PACE Activity Library
- Beginner-Level Activities
- Intermediate-Level Activities
- Advanced-Level Activities
- Maximizing PACE Therapy Success
- Adapting PACE for Different Aphasia Types
- Technology Integration
- Measuring Progress
- Long-Term Benefits and Outcomes
- Building Your PACE Therapy Journey
- Ready to Begin?
- FAQ: PACE Therapy
Understanding PACE Therapy: A Paradigm Shift in Aphasia Treatment
PACE (Promoting Aphasics' Communicative Effectiveness) represents a fundamental shift in how we approach aphasia rehabilitation.
Traditional speech therapy with a licensed SLP often emphasizes correcting specific linguistic deficits—working on word retrieval, grammar, or articulation in isolation. While these skills matter, PACE takes a broader, more functional perspective.
Anyone can act as a therapy partner, putting evidence-based practice like PACE into action at home and with minimal resources. At its core, PACE therapy operates on four essential principles:
1. Natural Information Exchange Communication occurs through genuine information sharing, not artificial drills. Participants have real reasons to communicate, creating authentic motivation and engagement.
2. Equal Participation Both the person with aphasia and their communication partner take turns being the sender and receiver of messages. This balanced dynamic mirrors real-world conversations and builds confidence on both sides.
3. Free Choice of Communication Channels Success is measured by effective message transmission, regardless of the method used. Speaking, writing, drawing, gesturing, pointing to pictures, or using technology—all are valid and valuable communication tools.
4. Feedback Based on Message Success Instead of correcting linguistic errors, feedback focuses on whether the intended message was successfully communicated. This positive reinforcement encourages risk-taking and creative problem-solving.
Who Can Benefit from PACE Therapy at Home?
PACE therapy has demonstrated remarkable effectiveness across various aphasia presentations and causes including stroke recovery, progressive conditions, and traumatic brain injuries:
Stroke Survivors
Expressive (Broca's) Aphasia: Individuals who understand well but struggle with speech production find PACE particularly liberating, as it validates their intact comprehension while providing alternative expression methods.
Mixed Aphasia: Those with both comprehension and expression challenges benefit from PACE's multimodal approach and reduced pressure for perfect linguistic performance.
Global Aphasia: Even individuals with severe language impairments can participate meaningfully when communication channels are opened beyond speech.
Progressive Aphasia
Primary Progressive Aphasia (PPA): As language abilities change over time, PACE helps individuals and families adapt their communication strategies, maintaining connection despite evolving challenges.
Frontotemporal Dementia: The flexible, creative nature of PACE accommodates the changing communication needs throughout disease progression.
Traumatic Brain Injury and Tumor Recovery
Cognitive-Communication Disorders: PACE addresses not just language deficits but also attention, memory, and executive function challenges that impact communication.
Acquired Aphasia: Whether from accident or medical intervention, PACE provides hope and practical strategies for rebuilding communication skills.
The Science Behind PACE: Why It Works
Research consistently demonstrates PACE therapy's effectiveness through several mechanisms:
Neuroplasticity Activation
By engaging multiple brain regions simultaneously—visual, motor, cognitive, and linguistic areas—PACE promotes neural reorganization and the development of alternative communication pathways.
Functional Communication Training
Unlike isolated skill practice, PACE activities mirror real-world communication demands, promoting transfer of learned strategies to daily life situations.
Confidence Building
Success-focused feedback creates positive associations with communication attempts, reducing anxiety and encouraging continued practice and risk-taking.
Partner Training
PACE naturally educates communication partners about effective support strategies, improving overall communication success within relationships and communities.
Setting Up Your Home PACE Practice
Creating an effective PACE practice environment requires minimal materials for in-home speech therapy for people with aphasia, but it does need some thoughtful preparation:
Essential Materials
Barrier Materials: Large books, folders, or cardboard screens to create visual barriers when needed
Image Collections: Family photos, magazine pictures, printed images from online sources, or commercial card sets
Drawing Supplies: Plain paper, pens, markers, or dry-erase boards
Real Objects: Household items, tools, toys, or personal belongings
Technology Tools: Tablets with drawing apps, communication apps, or picture libraries
Environmental Considerations
Comfortable Seating: Arrange chairs to facilitate easy eye contact and gesture visibility
Good Lighting: Ensure adequate illumination for reading, writing, and gesture recognition
Minimal Distractions: Choose quiet spaces away from television, radio, or high-traffic areas
Accessible Materials: Keep supplies within easy reach for spontaneous practice opportunities
Timing and Frequency
Short, Regular Sessions: 15-30 minute sessions work better than longer, infrequent practices
Energy-Appropriate Scheduling: Plan sessions when the person with aphasia feels most alert and energetic
Flexible Timing: Allow sessions to end naturally rather than forcing continuation when fatigue sets in
Comprehensive PACE Activity Library
Beginner-Level Activities: Building Foundation Skills
1. Enhanced Picture Description
Materials: Detailed photographs or illustrations depicting scenes, people, or events
Setup: Create a barrier between participants. The speaker examines an image while the listener cannot see it.
Execution: The speaker communicates everything they observe using any available method—speech, gestures, drawing, writing, or combinations thereof. The listener works to understand and may ask clarifying questions.
Variations:
Use family photos to add personal relevance
Start with simple images and progress to complex scenes
Include emotional content to practice expressing feelings
Use images that tell stories or show sequences
Therapeutic Benefits: Enhances word-finding abilities, promotes creative expression strategies, builds confidence in multimodal communication, and strengthens descriptive language skills.
2. Object Identification Challenge
Materials: Collection of 20-30 common household objects or printed object cards
Setup: Objects are hidden from one participant while the other examines them.
Execution: The speaker must convey the identity of each object without directly naming it. They might describe its function, demonstrate its use, draw its shape, or provide contextual clues.
Variations:
Group objects by category (kitchen items, tools, clothing)
Use objects with multiple functions to encourage creative descriptions
Include items with strong sensory associations
Progress from concrete objects to abstract concepts
Therapeutic Benefits: Strengthens semantic networks, encourages flexible thinking, develops circumlocution strategies, and builds tolerance for word-finding difficulties.
3. Strategic Yes/No Investigation
Materials: Picture cards or written concepts on paper slips
Setup: One person selects a card without showing it to their partner.
Execution: The guesser asks yes/no questions to identify the target item. The responder answers using gestures, facial expressions, writing, or speech—whatever feels most natural.
Variations:
Limit questions to specific categories (Is it living? Is it found indoors?)
Use topics of personal interest (family members, favorite foods, hobbies)
Include abstract concepts (emotions, experiences, memories)
Allow drawing or gesturing as part of responses
Therapeutic Benefits: Develops strategic questioning skills, enhances comprehension abilities, builds inference and deduction skills, and promotes interactive communication patterns.
Intermediate-Level Activities: Expanding Complexity
4. Navigation and Direction Giving
Materials: Simple maps, floor plans, or hand-drawn layouts of familiar spaces
Setup: Both participants have copies of the same map, but only one knows the destination.
Execution: The direction-giver guides their partner from a starting point to a specific destination using any communication method. The follower traces the route and asks for clarification when needed.
Variations:
Use maps of familiar places (home, neighborhood, grocery store)
Create treasure hunt scenarios with multiple stops
Include landmarks and reference points
Progress from simple layouts to complex multi-level buildings
Therapeutic Benefits: Strengthens spatial language, develops sequencing abilities, promotes clear and organized communication, and builds confidence in giving instructions.
5. Sequential Story Construction
Materials: Series of 4-6 pictures showing a logical sequence or story progression
Setup: The speaker arranges pictures in correct order while the listener has the same pictures in random arrangement.
Execution: The speaker describes the sequence, helping the listener arrange their pictures in matching order. Communication can include storytelling, describing connections between images, or explaining cause-and-effect relationships.
Variations:
Use personal photo sequences (vacation trips, family events)
Create fictional stories with provided images
Include problem-solving scenarios
Allow collaborative story creation
Therapeutic Benefits: Enhances narrative skills, develops logical sequencing abilities, strengthens cause-and-effect reasoning, and promotes sustained communication exchanges.
6. Collaborative Art Creation
Materials: Drawing paper and art supplies for both participants
Setup: One person examines a target image while the other prepares to draw.
Execution: The describer guides the artist in recreating the image through verbal instructions, gestures, and demonstrations. The artist asks questions and seeks clarification throughout the process.
Variations:
Use geometric shapes and patterns for precision practice
Include emotional or expressive elements in drawings
Create collaborative abstract art based on themes or feelings
Progress from simple line drawings to detailed illustrations
Therapeutic Benefits: Promotes detailed descriptive language, enhances spatial and directional vocabulary, builds collaborative communication skills, and develops patience with communication breakdowns.
Advanced-Level Activities: Real-World Application
7. Daily Experience Narrative
Materials: Prompt cards with time periods or activities (morning routine, grocery shopping, weekend plans)
Setup: Participants take turns sharing experiences with specific communication constraints.
Execution: The speaker describes their experience using limited verbal expression combined with gestures, drawings, or demonstrations. The listener actively engages through questions and clarification requests.
Variations:
Focus on emotional aspects of experiences
Include problem-solving elements (What did you do when...?)
Practice future planning and hypothetical situations
Incorporate social interactions and conversations
Therapeutic Benefits: Builds real-world communication confidence, develops personal narrative skills, strengthens emotional expression abilities, and promotes independence in social situations.
8. Persuasion and Argumentation
Materials: Prompt cards with debate topics, decision scenarios, or preference discussions
Setup: Present scenarios requiring persuasive communication or decision-making.
Execution: The speaker advocates for their position using all available communication tools while the listener asks challenging questions and seeks clarification of reasoning.
Variations:
Use personally relevant decisions (vacation destinations, meal choices)
Include moral or ethical dilemmas for deeper discussion
Practice consumer advocacy (returning items, making complaints)
Engage in hypothetical problem-solving scenarios
Therapeutic Benefits: Develops argumentative discourse skills, builds confidence in expressing opinions, strengthens reasoning and logic presentation, and prepares for real-world advocacy situations.
9. Interactive Problem Solving
Materials: Scenario cards describing everyday problems or challenges
Setup: Present complex situations requiring collaborative problem-solving.
Execution: Participants work together to understand the problem, generate solutions, and evaluate options using flexible communication strategies.
Variations:
Use real-life challenges faced by the person with aphasia
Include multi-step solutions requiring planning and organization
Practice emergency or urgent situation communication
Engage in creative problem-solving with multiple possible solutions
Therapeutic Benefits: Enhances collaborative communication, develops critical thinking expression, builds confidence in complex conversations, and strengthens real-world problem-solving abilities.
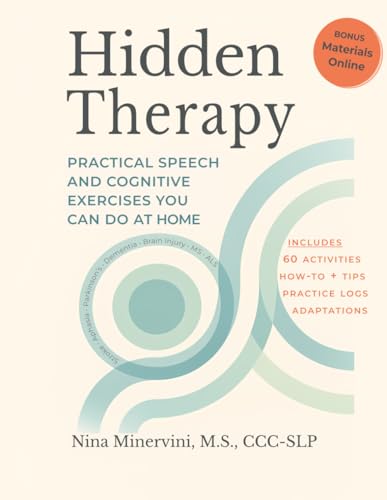
Hidden Therapy: Practical Speech and Cognitive Exercises You Can Do At Home
If you've found the PACE approach helpful, you'll love Hidden Therapy. This comprehensive activity book includes 60 therapeutic exercises specifically designed for home practice, with detailed adaptations for aphasia built into each activity.
- 60 Therapeutic Activities
- 11 Different Themes
- Support for Caregivers
- Bonus Materials Online
Maximizing PACE Therapy Success
For Communication Partners
Patience and Positivity: Allow time for message development and celebrate successful communication regardless of the method used. Avoid rushing or finishing sentences unless specifically requested.
Active Participation: Engage fully in both speaking and listening roles. Your genuine interest and participation directly impact the person with aphasia's motivation and success.
Flexible Support: Offer different types of assistance based on individual needs and preferences. Some people prefer minimal help, while others benefit from more active support.
Natural Feedback: Respond to the message content rather than the communication method. Focus on understanding and responding appropriately rather than correcting linguistic errors.
For Individuals with Aphasia
Embrace All Communication: Remember that successful message transmission matters more than perfect speech. Drawing, gestures, and technology are legitimate and valuable communication tools.
Practice Self-Advocacy: Communicate your preferences for support and feedback. Help your partners understand what assistance works best for you.
Celebrate Progress: Acknowledge improvements in communication effectiveness, confidence, and strategy use—not just speech clarity or word retrieval speed.
Stay Engaged: Continue practicing and challenging yourself with new activities and more complex communication situations.
Adapting PACE for Different Aphasia Types
Expressive Aphasia Adaptations
Emphasize alternative communication modalities
Provide extra time for message formulation
Focus on core message transmission over grammatical accuracy
Encourage use of key words and gestures together
Receptive Aphasia Modifications
Use visual supports and written backup
Simplify complex instructions initially
Check comprehension frequently through demonstration
Provide multiple examples and repetition when needed
Global Aphasia Accommodations
Start with very concrete, familiar topics
Use real objects whenever possible
Keep sessions shorter but more frequent
Celebrate any successful communication attempt
Technology Integration in PACE Therapy
Hand-held devices have become pervasive, and chances are you’ve got one in your pocket right now. Here’s how you can use your phone or tablet to augment or enhance PACE therapy.
Communication Apps
Symbol-based applications: Allow selection and combination of pictures or symbols
Text-to-speech programs: Support written communication when speaking is challenging
Drawing applications: Provide sophisticated tools for visual communication
Video calling platforms: Enable remote PACE practice with family and friends
Adaptive Equipment (AAC)
Communication boards: Low-tech options for gesture and pointing support
Voice amplifiers: Help with volume challenges during speech attempts
Specialized keyboards: Support written communication when hand function is affected
Eye-gaze systems: Provide communication access for individuals with severe motor impairments
Measuring Progress in PACE Therapy
Functional Communication Measures
Message Success Rate: Percentage of intended messages successfully communicated
Strategy Use Flexibility: Variety and appropriateness of communication methods employed
Communication Confidence: Self-reported comfort and willingness to engage in communication
Partner Satisfaction: Feedback from family and friends regarding communication effectiveness
Tracking Tools
Communication logs: Daily records of successful and challenging interactions
Video recordings: Periodic documentation of PACE sessions for progress review
Strategy checklists: Monitoring of communication method usage and effectiveness
Goal achievement records: Documentation of functional communication milestone attainment
Long-term Benefits and Outcomes
Research consistently demonstrates that PACE therapy produces lasting improvements in:
Functional communication effectiveness across various settings and partners
Confidence and willingness to engage in communication attempts
Quality of life and social participation through improved interaction abilities
Family and caregiver satisfaction with communication success
Independence in daily communication tasks and social situations
Building Your PACE Therapy Journey
Recovery from aphasia is rarely linear, and progress often comes in waves rather than steady upward climbs. PACE therapy acknowledges this reality by focusing on functional success rather than perfect performance. \
Every successful message—whether spoken, drawn, gestured, or written—strengthens neural pathways and builds confidence for future communication attempts.
The beauty of PACE lies in its recognition that communication is fundamentally about human connection.
When we remove the pressure for perfect speech and instead celebrate successful message sharing, we open doors to meaningful interaction that might otherwise remain closed.
Whether you're just beginning your aphasia recovery journey or seeking to enhance existing communication strategies, PACE therapy offers hope, practical tools, and a pathway to reconnection.
Through consistent practice, patient support, and celebration of all communication successes, individuals with aphasia can rebuild their voice and reclaim their place in conversations that matter.
Remember: your message matters more than the method you use to share it.
PACE therapy helps you discover and develop the communication strategies that work best for you, building bridges to the connections and conversations that enrich life and restore confidence in your communicative abilities.
Ready to Begin Your PACE Therapy Journey?
Don't let aphasia define your communication story. If you or a loved one is ready to explore the transformative power of PACE therapy and other evidence-based speech treatment approaches, professional guidance can make all the difference in your recovery journey.
Contact Nina today to discover how personalized, research-backed speech therapy can help you rebuild confidence and reclaim your voice. Specializing in aphasia recovery and functional communication strategies, Nina provides compassionate, expert care tailored to your unique needs and goals.
Serving communities in Lantana, Lake Worth, Boynton Beach, and coastal Palm Beach County, Nina brings evidence-based practice directly to you, whether online or through convenient home visits.
Your communication breakthrough is waiting. Take the first step toward reconnecting with the conversations and relationships that matter most.
Get in Touch!
Frequently Asked Questions: PACE Therapy for Aphasia and Stroke
1) What is PACE therapy?
PACE stands for Promoting Aphasics’ Communicative Effectiveness. It is a conversational approach that helps people communicate using any effective channel, including speech, gesture, writing, drawing, or AAC. The goal is successful message exchange in real-life situations.
2) Who can benefit from PACE therapy?
Adults with aphasia after stroke or brain injury are the most common candidates. PACE can also support people with apraxia of speech or dysarthria when communication breakdowns make everyday conversations difficult.
3) How does a typical PACE session work?
Therapist and client take turns sending and receiving messages with a shared purpose, like describing a picture or solving a task. The focus is on getting the idea across, not perfection, and cues are added as needed to help the message succeed.
4) Can PACE therapy be done at home?
Yes. With guidance from a speech-language pathologist, families can practice short, structured activities at home and embed PACE principles into daily routines like meals, phone calls, and planning the day.
5) What materials do I need to practice PACE?
Simple tools work well. Picture cards, everyday objects, a notepad and pen, a whiteboard, or a communication app are often enough to practice sending and receiving messages in different ways.
6) How can family and caregivers help?
Caregivers can model slow, supportive conversations, ask clear questions, accept any successful communication method, and give time for responses. They can also help set up short daily practice sessions and track what works best.
7) How is PACE different from drill-based speech therapy?
Drill approaches often target specific sounds or words in isolation. PACE centers on natural conversation with shared information needs and encourages any strategy that makes the message succeed, which can generalize better to real life.
8) Does PACE work for severe aphasia or apraxia?
Yes, with adaptations. For severe aphasia or apraxia, sessions may rely more on gestures, drawing, yes or no responses, written keywords, or AAC tools, with frequent cues and smaller targets that build success step by step.
9) How do we measure progress with PACE?
Progress can be tracked by time to get messages across, the number of successful exchanges, reduced need for cues, and improvements in participation and confidence during everyday conversations reported by the client and family.
10) What role do AAC and technology play in PACE?
AAC fits naturally into PACE because any effective mode counts. Low-tech boards, texting, speech-generating apps, and photo libraries can all support message success and help conversations move forward.
11) How often should I practice PACE?
Daily practice in short, focused sessions works well. Many people aim for 10 to 20 minutes once or twice a day, plus quick opportunities during routine activities.
12) Why is it called PACE and is the name outdated?
The method was named when the term “aphasics” was common in clinical writing. Today many prefer person-first language such as person with aphasia. The approach itself remains useful, and you can refer to it as the PACE approach for people with aphasia.